Performing a physical assessment
Table of Contents
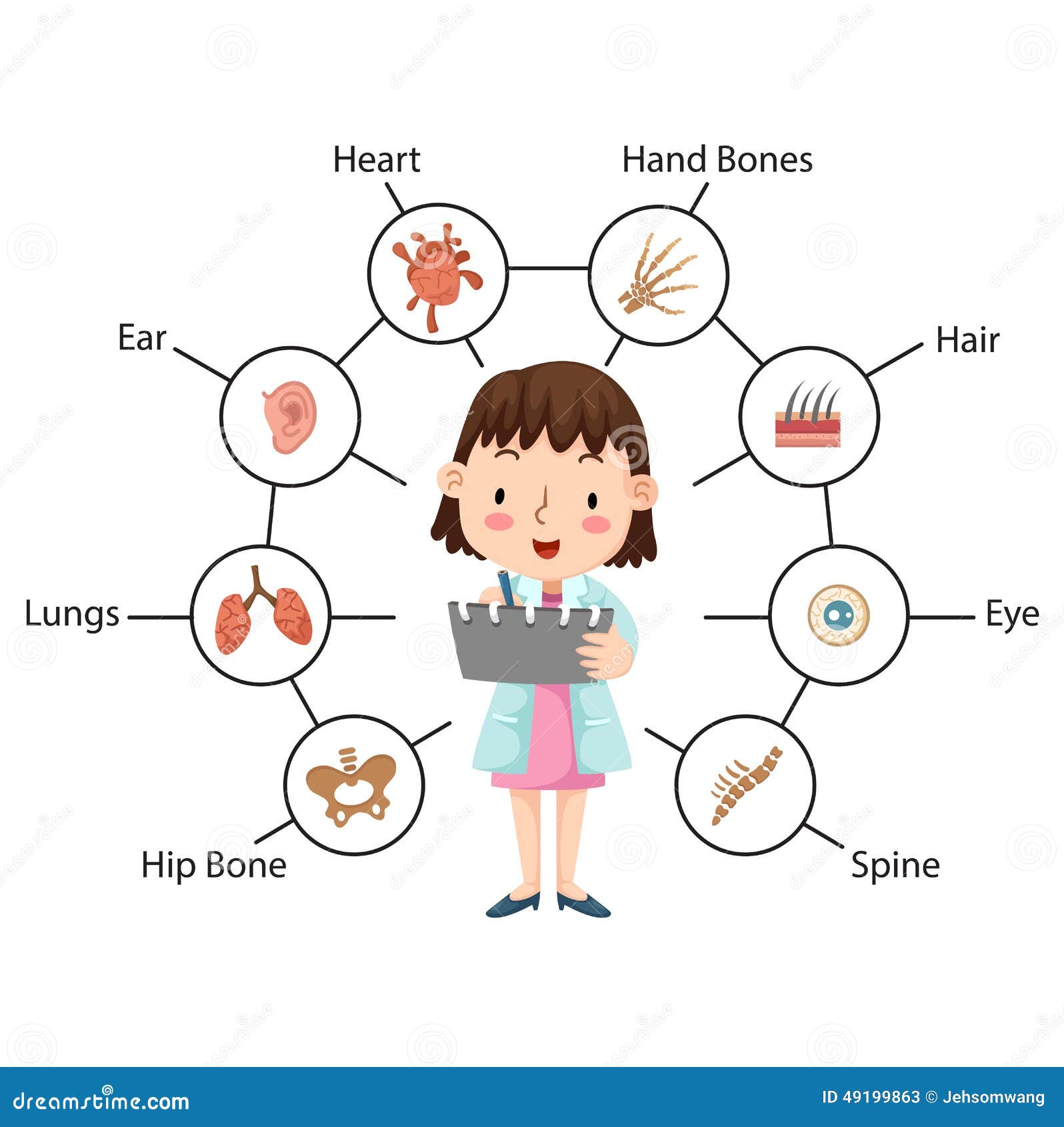
The physical assessment lies at the heart of clinical practice, a crucial skill wielded by healthcare professionals to decipher the body’s language and uncover potential health concerns. It’s a multi-faceted dance, weaving together observation, palpation, percussion, and auscultation to create a holistic picture of the patient’s condition. Whether in the sterile environment of a hospital room or the familiar comfort of a patient’s home, mastering this art of performing a physical assessment empowers you to initiate effective interventions, personalize care, and ultimately guide patients toward optimal health.
Preparing for the Physical Assessment
Think of a physical assessment not as a sterile procedure but as a delicate dance between you and the patient. This intricate tango requires meticulous preparation before the music even begins. Let’s explore the key steps to ensure a smooth and informative assessment:
1. Knowledge is Power: Gather Information:
Before stepping into the room:
- Arm yourself with knowledge.
- Review the patient’s medical history, medications, and allergies.
- Look for red flags, potential areas of focus, and any cultural considerations.
This pre-assessment equips you to tailor your approach, anticipate concerns, and avoid unnecessary discomfort.
2. Setting the Stage: Create a Welcoming Environment:
Imagine yourself setting the scene for a beautiful dance. Ensure the room is comfortably warm, well-lit, and has adequate space for manoeuvring. Offer blankets for warmth and ensure privacy by closing curtains or doors. Remember, creating a comfortable environment fosters trust and facilitates open communication.
3. Introducing Yourself: The First Steps of the Dance:
First impressions matter! Introduce yourself warmly and professionally. Explain the purpose of the assessment in clear, concise language and obtain informed consent. Briefly explain what to expect and answer any questions they may have. Remember, this is a partnership, and setting the tone with respect and empathy is crucial.
4. Getting Ready to Move: Essential Equipment:
Gather the necessary tools for your dance – a stethoscope, thermometer, blood pressure cuff, and other equipment specific to the patient’s needs. Ensure everything is functioning properly and readily accessible. Remember, organization allows for a smoother flow and minimizes disruptions.
5. Hygiene and Safety: Setting the Boundaries:
Wash your hands thoroughly before and after the assessment. Wear appropriate personal protective equipment (PPE) as needed. Be mindful of the patient’s safety and comfort throughout the examination. Remember, hygiene and safety are essential for both you and the patient.
6. Documentation: Capturing the Steps:
Prepare your documentation tools – paper charts or electronic health records. Jot down key observations and findings as you proceed. Remember, accurate and timely documentation ensures continuity of care and serves as a reference point for future assessments.
You create the foundation for a successful and informative dance by meticulously preparing for the physical assessment. This initial phase demonstrates your professionalism, builds trust with the patient, and allows you to enter the assessment focused and ready to gather valuable insights into their health status. Remember, preparation is not just a step; it’s the opening act that sets the stage for a meaningful and impactful clinical encounter.
Palpitation
Palpation stands out as a unique and powerful tool within the symphony of physical assessment. It’s not just about touching the body; it’s about listening to its whispers, deciphering its unspoken language through the gentle pressure of your fingertips and palms. When performed with skill and sensitivity, this tactile dance can unveil hidden clues, confirm suspicions, and paint a vivid picture of the patient’s health.
The Layers of Touch:
Palpation is a multi-layered art, each level revealing different aspects of the body’s story:
- Superficial palpation: Imagine your fingertips dancing across the skin, assessing temperature, moisture, texture, and turgor. Is the skin warm and dry or cool and clammy? Is it smooth and elastic, or rough and fragile? These subtle details can hint at dehydration, inflammation, or nutritional deficiencies.
- Deep palpation: Delve deeper with your palms, pressing gently to assess muscle tone, tenderness, and organomegaly. Does a muscle feel tense and tight, suggesting potential strain? Is there a tender spot in the abdomen, indicating possible inflammation? By palpating deeper, you gain insights into the condition of muscles, organs, and underlying structures.
- Specific area palpation: Each body system has its unique palpation techniques. Feeling the thyroid for nodules, checking lymph nodes for enlargement, or palpating the abdomen for masses requires specific manoeuvres and interpretations. Mastering these techniques allows you to assess specific concerns with greater accuracy.
Beyond the Technique
Remember, palpation is not just a mechanical exercise; it’s a conversation:
- Communicate with the patient: Explain what you’re doing and why, and ask about any discomfort they may experience. This builds trust and allows them to participate in the physical assessment.
- Be mindful of pressure and respect: Use gentle yet firm pressure, respecting the patient’s comfort and cultural sensitivities. Always ask permission before touching sensitive areas.
- Observe and interpret: Don’t just feel; observe the patient’s reaction to palpation. Is there wincing, guarding, or any changes in facial expression? These subtle cues can be as valuable as the physical findings themselves.
The Power of Touch:
Skilled palpation can:
- Confirm suspicions: A tender and swollen abdomen during palpation can confirm your initial suspicion of appendicitis.
- Uncover hidden clues: A small, hard mass felt in the thyroid during palpation might lead to further investigation for possible nodules.
- Guide further interventions: Identifying muscle tightness through palpation might inform the need for physical therapy or stretching exercises.
Remember, palpation is not a standalone act; it’s a crucial piece of the physical assessment puzzle. Integrating it with other techniques like observation, percussion, and auscultation gives you a comprehensive understanding of the patient’s health status. Master the art of palpation; you’ll unlock a world of hidden information, allowing you to become a more perceptive and effective healthcare provider.
Percussion
Imagine tapping on a drum, listening to the reverberations and interpreting the sounds to understand the instrument’s condition. Similarly, percussion, another pillar of physical assessment, involves tapping the body to unveil hidden messages about its health. You can listen to the body’s internal melodies through this rhythmic dance of fingertips and hammers, gaining valuable insights into organ function, fluid levels, and potential abnormalities.
The Symphony of Sounds:
Percussion utilizes two main techniques:
- Indirect percussion: Imagine your fingertips gently drumming on the chest or abdomen. This light tapping creates vibrations that travel through tissues and reflect, producing sounds like resonance (hollow), dullness (flat), or tympany (drum-like). Resonance suggests air-filled structures like lungs, while dullness indicates fluid or solid organs. Tympany might point towards gas in the intestines.
- Direct percussion: For targeted examination, a percussion hammer comes into play. Tapping specific areas like the chest wall or the border of the liver releases specific sounds that offer clues about underlying structures. Dullness over the lungs might indicate pneumonia, while hyperresonance could suggest pneumothorax (collapsed lung).
Beyond the Technique:
While mastering the technique is crucial, remember percussion is about more than sounds:
- Positioning matters: Ensure proper positioning of the patient and your hand (for indirect percussion) or the hammer (for direct percussion) to elicit accurate sounds.
- Interpretation is key: Analyze the sounds in context. Consider other findings from observation, palpation, and the patient’s history to accurately interpret the meaning of resonance, dullness, or tympany.
- Communication is essential: Explain the procedure and potential discomfort beforehand and observe the patient’s reaction during percussion. Address any concerns they might have.
The Power of Listening:
Skilled percussion can:
- Assess lung function: Identify fluid in the lungs (pleural effusion) or air in the pleural space (pneumothorax) by interpreting changes in resonance and dullness.
- Evaluate organ size and function: Determine liver or spleen enlargement by listening for changes in percussion sounds over their respective areas.
- Detect potential issues: Identify ascites (fluid in the abdomen) by detecting shifting dullness during percussion in different positions.
Remember, percussion is not a solo performance; it’s a harmonious collaboration. Integrating it with other assessment techniques creates a comprehensive picture of the patient’s health. Master the art of percussion, and you’ll become a master listener, deciphering the body’s hidden rhythms and providing invaluable insights for diagnosis and treatment.
Auscultation
Imagine pressing your ear to a seashell, captivated by the symphony of the ocean within. In physical assessment, auscultation serves as your seashell, amplifying the hidden sounds of the body to reveal vital clues about its health. Through the skilled use of a stethoscope, you embark on a journey of listening and deciphering the whispers of the heart, lungs, and other vital organs, painting a vivid picture of their function and potential issues.
Tuning into the Body’s Orchestra:
Auscultation involves placing the stethoscope on specific areas and listening attentively to the sounds produced:
- The heart: Imagine listening to a beating drum. Listen for the normal rhythm and rate, extra sounds like murmurs or clicks, and any changes in intensity or quality. These can indicate potential issues like valve problems or arrhythmias.
- The lungs: Think of listening to the wind rustling through leaves. Listen for normal breath sounds like inspiration and expiration, and be alert for abnormal sounds like wheezing, crackles, or rhonchi. These can suggest conditions like asthma, pneumonia, or lung fluid.
- The abdomen: Imagine the gurgling of a running stream. Listen for bowel sounds, their frequency and character. Absent or high-pitched sounds can indicate potential bowel obstruction, while hyperactive sounds might suggest inflammation.
- Blood vessels: Focus on the whooshing sound of blood flow. Identify bruits and abnormal swishing sounds that can indicate narrowed arteries or other vascular issues.
Beyond the Stethoscope:
Remember, auscultation is more than just listening through a cold metal device:
- Positioning matters: Ensure proper patient positioning for optimal sound acquisition. Consider age, limitations, and comfort when positioning the stethoscope.
- Be an active listener: Focus intently on the sounds, filtering out ambient noise. Use different pressures and angles to elicit specific sounds like faint murmurs.
- Interpret in context: Analyze the sounds in conjunction with other assessment findings, the patient’s history, and their symptoms. Don’t rely on auscultation alone to reach conclusions.
The Power of Amplification:
Skilled auscultation can:
- Diagnose heart problems: Identify valvular issues, arrhythmias, and pericarditis based on abnormal heart sounds.
- Detect lung conditions: Recognize asthma, pneumonia, and pleural effusions by interpreting abnormal breath sounds.
- Uncover bowel issues: Identify potential bowel obstruction or inflammation based on changes in bowel sounds.
- Monitor vascular health: Detect aneurysms, arteriovenous malformations, and other vascular problems by listening to blood flow sounds.
Remember, auscultation is not a standalone act; it’s a vital piece of the diagnostic puzzle. Integrating it with other assessment techniques gives you a comprehensive understanding of the patient’s health status. Master the art of listening with your stethoscope, and you’ll become a skilled detective, unveiling hidden clues and guiding patients towards improved health.
Beyond the Technique:
Remember, the physical assessment is not just about technical skills; it’s also about communication and empathy:
- Engage the patient: Ask open-ended questions, listen actively to their concerns, and explain your findings in understandable language.
- Be respectful: Treat the patient with dignity and respect throughout the assessment.
- Maintain confidentiality: Ensure the privacy and confidentiality of all information obtained during the assessment.
Putting it All Together:
By skillfully weaving together the four pillars of assessment, you gain valuable insights into the patient’s health status. This information forms the foundation for:
- Diagnosing potential health problems: The assessment findings can help you identify potential diagnoses and guide further investigations.
- Developing a personalized care plan: Based on the assessment findings, you can tailor interventions and treatment plans to address the patient’s needs.
- Monitoring progress: Regularly reassessing the patient allows you to track their response to treatment and adjust the care plan as needed.

Remember, the physical assessment is a dynamic process, not a static event. It’s an ongoing conversation between you and the patient, continuously evolving as their condition changes and new information emerges. Mastering this skill empowers you to become a more effective and compassionate healthcare provider, making a tangible difference in the lives of your patients.
Additional Resources:
- National League for Nursing (NLN): https://www.nln.org/
- American Nurses Association (ANA): [https://www.nursing
Conclusion
The physical assessment, a cornerstone of clinical practice, empowers healthcare professionals to decipher the body’s language and uncover potential health concerns. Through meticulous preparation, mastering the four techniques of inspection, palpation, percussion, and auscultation, and prioritizing communication and empathy, you can effectively dance with your patients, gathering valuable insights to diagnose, personalize care, and ultimately guide them towards optimal health. Remember, this is a continuous conversation, evolving with each encounter as you strive to become a more effective and compassionate healthcare provider.