Table of Contents
Nursing stands as the cornerstone of healthcare delivery worldwide. Nurses are the frontline caregivers, the patient advocates, the critical thinkers, and the compassionate presence during times of vulnerability and crisis. Their dedication is undeniable, yet the very nature of their profession exposes them to significant stressors that profoundly impact their overall health. This brings us to the crucial, intertwined concepts of nurse well-being and burnout.
Understanding this dynamic is not just an occupational health issue; it is fundamental to patient safety, healthcare quality, and the sustainability of the entire healthcare system. Ignoring the state of nurse well-being and burnout carries dire consequences for nurses themselves, the patients they serve, and the organizations they work for.
The dialogue surrounding nurse well-being and burnout has intensified in recent years, particularly highlighted by the unprecedented pressures of global health crises like the COVID-19 pandemic. However, the problem predates the pandemic, rooted deeply in systemic issues within healthcare environments.
This guide shines a light on the complex landscape of nurse well-being and burnout, exploring its definitions, causative factors, far-reaching consequences, and, most importantly, evidence-based strategies for mitigation and prevention. Addressing nurse well-being and burnout requires a multi-faceted approach, demanding commitment from individuals, organizations, and policymakers alike.
Defining the Terms: Nurse Well-Being vs. Burnout
Before exploring solutions, it’s essential to clearly define the key terms at the heart of this discussion:
- Nurse Well-Being: This refers to a holistic state encompassing nurses’ physical, mental, emotional, and social health. It’s characterized by feelings of satisfaction, engagement, resilience, purpose, and safety in the work environment. High nurse well-being means nurses feel valued, supported, and equipped to handle the demands of their jobs without compromising their own health. It’s a positive state that allows nurses to thrive, not just survive. Promoting nurse well-being and burnout prevention are intrinsically linked goals.
- Nurse Burnout: As defined by researchers like Christina Maslach, burnout is a psychological syndrome emerging as a prolonged response to chronic interpersonal stressors on the job. It comprises three key dimensions:
- Emotional Exhaustion: Feeling emotionally drained, depleted, and unable to give more on a psychological level. This is often the first sign recognized in discussions about nurse well-being and burnout.
- Depersonalization (or Cynicism): Developing a detached, callous, or cynical attitude towards patients, colleagues, and the job itself. This is a coping mechanism that tragically distances the nurse from the compassionate core of their profession.
- Reduced Sense of Personal Accomplishment: Feeling incompetent, ineffective, and lacking achievement in one’s work. Nurses may feel their efforts make no difference, leading to disillusionment.
It is critical to understand that nurse well-being and burnout exist on a spectrum. Burnout represents the negative endpoint, resulting from the erosion of well-being due to unmanaged, chronic workplace stress. Therefore, strategies aimed at improving nurse well-being and burnout outcomes must focus on both enhancing positive factors (well-being) and reducing negative factors (stressors leading to burnout).
The Pervasive Problem: Why Nurses are Vulnerable
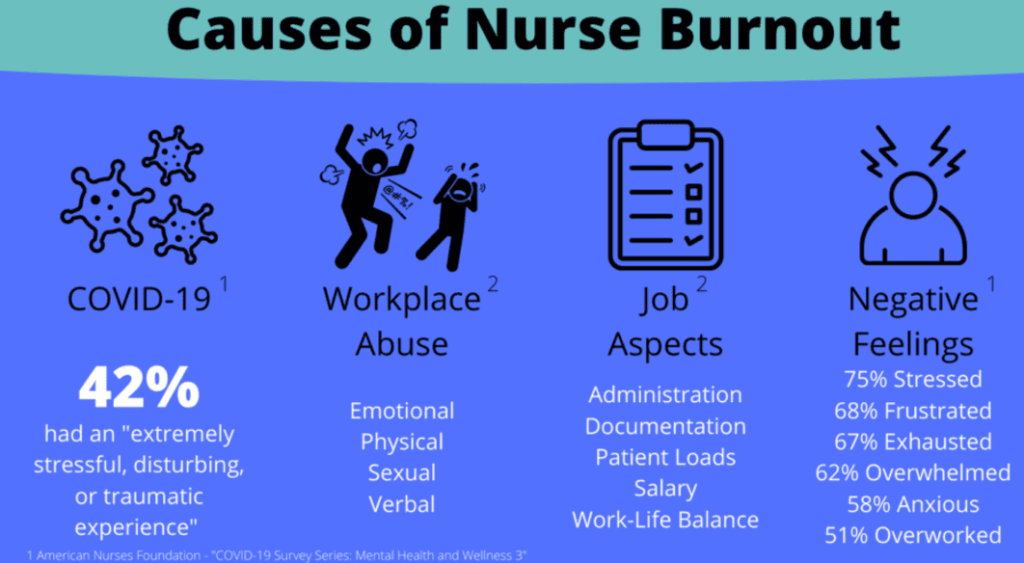
The nursing profession carries inherent stressors that make discussions about nurse well-being and burnout particularly pertinent. Nursing burnout statistics show several factors contribute to nurses’ vulnerability:
- High Workload and Pace: Nurses often juggle care for multiple patients, many with complex needs, under significant time pressure. Inadequate staffing levels exacerbate this, stretching resources thin and intensifying the workload, directly impacting nurse well-being and burnout.
- Emotional Labor: Nurses constantly manage their own emotions while dealing with patients’ and families’ pain, fear, grief, and anger. This emotional toll is immense and a key factor contributing to poor nurse well-being and burnout statistics.
- Long Work Hours and Shift Work: 12-hour shifts, night shifts, rotating shifts, and mandatory overtime disrupt circadian rhythms, leading to fatigue, sleep deprivation, and increased risk of errors. This pattern is detrimental to nurse well-being and burnout levels.
- Exposure to Trauma and Suffering: Regularly witnessing trauma, death, and critical illness takes a psychological toll, potentially leading to compassion fatigue, secondary traumatic stress, and burnout. Addressing this exposure is vital for nurse well-being and burnout initiatives.
- Lack of Control and Autonomy: Feeling powerless over staffing decisions, work processes, or patient assignments can lead to frustration and feelings of inadequacy, negatively influencing nurse well-being and burnout.
- Workplace Violence and Incivility: Nurses face alarmingly high rates of verbal abuse and physical assault from patients and families, as well as incivility or bullying from colleagues and superiors. A toxic work environment is a major driver of poor nurse well-being and burnout.
- Moral Distress: Situations where nurses know the ethically correct action to take but are constrained from doing so by institutional policies, resource limitations, or conflicting values cause significant internal conflict, contributing negatively to nurse well-being and burnout.
- Systemic Pressures: Budget cuts, increased documentation demands, focus on metrics over patient care, and lack of administrative support create an environment where nurse well-being and burnout become systemic problems rather than individual failings.
Understanding these contributing factors is the first step in developing effective strategies to improve nurse well-being and burnout.
The Consequences of Poor Nurse Well-Being and Burnout
The impact of neglecting nurse well-being and burnout extends far beyond the individual nurse, creating damaging ripples throughout the healthcare ecosystem.
Consequences for Nurses:
- Mental Health Issues: Increased rates of anxiety, depression, post-traumatic stress disorder (PTSD), substance use disorders, and tragically, suicidal ideation. Addressing the well-being and burnout of nurses is a mental health imperative.
- Physical Health Problems: Chronic stress contributes to fatigue, insomnia, headaches, gastrointestinal issues, cardiovascular disease, and weakened immune function. The physical toll underscores the urgency of improving nurse well-being and burnout.
- Decreased Job Satisfaction: Burned-out nurses often feel disillusioned with their chosen profession, leading to apathy and reduced engagement. This is a direct outcome when nurse well-being and burnout are poorly managed.
- Increased Intention to Leave: Burnout is a primary predictor of nurses leaving their current job or the profession entirely. High turnover rates are a clear symptom of unaddressed nurse well-being and burnout.
Consequences for Patients:
- Compromised Patient Safety: Fatigued, stressed, and emotionally exhausted nurses are more prone to making medical errors, including medication errors, procedural mistakes, and lapses in monitoring. Patient safety is directly linked to nurse well-being and burnout.
- Reduced Quality of Care: Depersonalization can lead to less compassionate care, poorer communication, and decreased attention to patient needs. Optimal patient outcomes depend on positive nurse well-being and burnout management.
- Lower Patient Satisfaction: Patients can often perceive when their caregivers are stressed or detached, leading to lower satisfaction scores and a negative care experience.
- Increased Risk of Infections: Studies have linked nurse burnout to higher rates of hospital-acquired infections, possibly due to lapses in adherence to protocols when staff are overwhelmed. This highlights a critical link between nurses’ well-being and burnout and basic safety measures.
Consequences for Healthcare Organizations:
- High Turnover Costs: Replacing a nurse is expensive, involving costs for recruitment, hiring, orientation, and lost productivity. Persistent issues with nurses’ well-being and burnout drive these costs up significantly.
- Increased Absenteeism: Burned-out nurses are more likely to call in sick, further straining staffing levels and increasing the workload on remaining staff, creating a vicious cycle related to nurse well-being and burnout.
- Decreased Productivity and Efficiency: A disengaged and exhausted workforce is less productive, impacting overall organizational performance. Investing in the prevention of nurses’well-being and burnout prevention is an investment in efficiency.
- Damage to Reputation: High turnover rates and reports of poor working conditions can damage an organization’s reputation, making it harder to attract and retain skilled nurses. Addressing nurse well-being and burnout proactively protects organizational image.
Consequences for the Healthcare System:
- Exacerbation of Nursing Shortages: High rates of burnout contribute significantly to nurses leaving the profession, worsening existing shortages and threatening the system’s capacity to provide care. The future of healthcare depends on tackling nurse well-being and burnout.
- Increased Healthcare Costs: Turnover, medical errors, and lower productivity all contribute to increased overall healthcare expenditures. Managing the well-being and burnout of nurses can contribute to cost containment.
- Strain on Remaining Workforce: As nurses leave, the burden on those who remain increases, perpetuating the cycle of stress and burnout. This systemic strain underscores the need for system-wide solutions for nurse well-being and burnout.
The evidence is clear: nurse well-being and burnout is not a peripheral issue but a central challenge with profound implications at every level of healthcare.
Strategies for Cultivating Well-Being and Combating Burnout
Addressing the complex issue of nurses’ well-being and burnout requires a comprehensive, multi-level approach. While individual coping strategies are important, sustainable change necessitates a strong focus on organizational and systemic interventions.
Organizational and Systemic Strategies (The Foundation):
These strategies target the work environment and system structures that contribute to poor nurse well-being and burnout.
- Ensure Adequate Staffing Levels: Implementing evidence-based staffing ratios and acuity-based models is paramount. Safe staffing reduces excessive workload, a primary driver of negative nurse well-being and burnout outcomes.
- Foster Supportive Leadership: Train managers and leaders to be empathetic, communicative, and responsive to staff concerns. Supportive leadership creates psychological safety and is crucial for improving the well-being and burnout of nurses.
- Promote visible and accessible leadership.
- Actively listen to and act upon nurse feedback.
- Recognize and reward nurses’ contributions.
- Cultivate a Positive Work Culture: Promote teamwork, respect, and civility. Implement zero-tolerance policies for workplace violence and bullying. A healthy culture is fundamental to positive nurse well-being and burnout.
- Promote Work-Life Balance:
- Offer flexible scheduling options where feasible.
- Ensure nurses take uninterrupted breaks.
- Minimize mandatory overtime.
- Encourage use of paid time off. Policies supporting balance are key for nurse well-being and burnout.
- Provide Robust Mental Health Support: Offer easily accessible and confidential mental health resources, such as Employee Assistance Programs (EAPs), counseling services, peer support programs, and stress management workshops. Normalizing help-seeking is vital for addressing the well-being and burnout of nurses.
- Empower Nurses: Increase nurse autonomy and control over their practice through shared governance models and involvement in decision-making processes that affect their work. Empowerment positively impacts nurse well-being and burnout.
- Invest in Resources and Efficient Workflows: Ensure nurses have the necessary equipment, supplies, and technology to do their jobs effectively. Streamline documentation processes to reduce administrative burden. Resource adequacy influences nurses’ well-being and burnout.
- Implement Debriefing and Support Mechanisms: Provide opportunities for structured debriefing after critical incidents or traumatic events to help nurses process their experiences. This support is essential for managing the emotional toll contributing to poor nurse well-being and burnout.
- Fair Compensation and Benefits: Ensure competitive wages and comprehensive benefits packages that reflect the value and demands of the nursing profession. Feeling fairly compensated impacts perceptions of nurses’ well-being and burnout.
Individual Strategies (Self-Care and Resilience Building):
While systemic change is primary, individual strategies can help nurses cope with stress and build resilience. Organizations should support and facilitate these.
- Practice Mindfulness and Stress Reduction: Techniques like deep breathing, meditation, and yoga can help manage acute stress responses.
- Prioritize Physical Health: Emphasize adequate sleep, healthy nutrition, and regular exercise as foundational elements of well-being. Physical health strongly influences nurses’ well-being and burnout.
- Set Healthy Boundaries: Learn to separate work life from personal life, disconnect during off-hours, and protect personal time. Boundary setting is crucial for managing nurse well-being and burnout.
- Build Social Support Networks: Connect with supportive colleagues, mentors, friends, and family. Peer support groups can be particularly beneficial for sharing experiences related to the well-being and burnout of nurses.
- Engage in Meaningful Activities Outside Work: Pursue hobbies and interests that bring joy and relaxation, providing an outlet from work stressors. This balance is important for nurses’ well-being and burnout.
- Develop Self-Compassion: Acknowledge the difficulty of the job and treat oneself with kindness, especially during challenging times. Self-compassion helps buffer against the negative effects associated with nurses’ well-being and burnout.
- Seek Professional Help When Needed: Recognize the signs of burnout and distress early and utilize available mental health resources without stigma. Proactive help-seeking is key to addressing nurse well-being and burnout.

It’s crucial to reiterate that individual strategies should complement, not replace, organizational responsibility for creating a healthy work environment that fosters positive nurses’ well-being and burnout outcomes. Placing the burden solely on nurses to “be more resilient” while ignoring systemic problems is ineffective and unjust.
The Role of Education and Research in Nurse Well-Being and Burnout
Academia and research play a vital role in advancing our understanding and management of nurse well-being and burnout.
- Integrating into Curricula: Nursing schools should incorporate comprehensive education on stress management, resilience, self-care, and the systemic factors contributing to nurses’ well-being and burnout into their curricula. Preparing future nurses for the realities of the profession is essential.
- Ongoing Research: Continued research is needed to:
- Identify emerging risk factors for poor nurse well-being and burnout.
- Evaluate the effectiveness of different intervention strategies.
- Understand the long-term impacts of nurse well-being and burnout on individuals and the healthcare system.
- Explore variations in nurse well-being and burnout across different specialties, settings, and demographics.
- Dissemination of Findings: Research findings must be effectively communicated to healthcare leaders, policymakers, and practicing nurses to inform evidence-based practices aimed at improving nurse well-being and burnout.
Many students undertake research papers about nurse well-being and burnout to better understand these complex issues and contribute to the knowledge base. The depth of the topic means that sometimes students find themselves seeking help with papers on nurse well-being and burnout to navigate the extensive literature and data effectively. This academic exploration is crucial for developing nuanced solutions.
Nursing Papers is the go-to platform for authentic and impactful nursing research papers. We handle all types of nursing papers including research papers, essays, term papers, assignments, case studies, thesis and dissertations. Our service covers topic suggestion, paper writing, proofreading, editing, formatting and plagiarism removal.
A Collective Responsibility: Moving Towards a Sustainable Future
Improving nurse well-being and burnout outcomes is not solely the responsibility of hospital administrators or individual nurses. It requires a collective effort from all stakeholders:
- Healthcare Organizations: Must prioritize creating psychologically safe and supportive work environments through systemic changes, investing in resources, and genuinely valuing their nursing staff. Their commitment is foundational to addressing nurses’ well-being and burnout.
- Nurse Leaders: Must advocate for their staff, model healthy behaviors, foster open communication, and implement policies that support nurse well-being and burnout prevention.
- Individual Nurses: Must prioritize self-care, utilize available resources, support their colleagues, and advocate for necessary changes within their workplaces. Recognizing the importance of nurse well-being and burnout personally is key.
- Policymakers: Must address broader issues like safe staffing legislation, funding for mental health resources for healthcare workers, and regulations to curb workplace violence. Policy plays a critical role in shaping the environment affecting nurse well-being and burnout.
- Educators: Must prepare nursing students for the challenges ahead and equip them with knowledge and skills related to nurse well-being and burnout.
- The Public: Must recognize the demanding nature of nursing and show respect and appreciation for the nursing workforce, fostering a culture that values their contribution and understands the pressures related to the well-being and burnout of nurses.
Conclusion: Prioritizing Those Who Care for Us
Nurse well-being and burnout represents one of the most significant challenges facing the healthcare sector today. The high rates of burnout, driven by demanding work conditions and systemic stressors, threaten the health of individual nurses, the safety of patients, the stability of healthcare organizations, and the sustainability of the entire system. Addressing nurse well-being and burnout is not optional; it is an ethical and operational imperative.
We must move beyond acknowledging the problem to implementing comprehensive, evidence-based solutions. This requires a fundamental shift towards creating work environments where nurses feel safe, supported, valued, and empowered. While individual resilience is important, the primary focus must be on systemic changes that tackle the root causes of chronic stress and exhaustion. Investing in nurses’ well-being and burnout prevention strategies is an investment in high-quality patient care and the future of nursing.
The path forward demands commitment, collaboration, and sustained effort from everyone involved. Prioritizing the well-being and burnout of nurses safeguards the health of a vital workforce but also ensure the delivery of compassionate, safe, and effective care for all. Let us commit to fostering environments where nurses can thrive, ensuring the enduring strength of the profession that cares for us all. The conversation about nurse well-being and burnout must continue, leading to tangible actions that make a lasting difference. Ultimately, the health of our nurses reflects the health of our healthcare system; protecting nurse well-being and burnout mitigation efforts protects us all.