Table of Contents
Nursing is consistently ranked among the most demanding professions globally. It requires a unique blend of clinical expertise, profound empathy, physical stamina, and emotional resilience. Nurses stand on the front lines of healthcare, providing critical care, comfort, and advocacy for patients often during their most vulnerable moments. While inherently rewarding, this demanding role inevitably takes a toll, making the conversation around nurses’ mental health not just relevant, but absolutely critical.
Ignoring the psychological well-being of this vital workforce has profound implications not only for the nurses themselves but also for patient safety and the overall health of our healthcare systems. Prioritizing nurses’ mental health must become a fundamental aspect of healthcare culture. Promoting mental wellbeing in nursing education and practice is critical to healthcare.
The daily realities of nursing involve exposure to trauma, suffering, and death, coupled with high-pressure situations, complex ethical dilemmas, long hours, and often, challenging workplace dynamics. The cumulative effect of these stressors can significantly erode nurses’ mental health, leading to conditions like burnout, compassion fatigue, anxiety, depression, and even post-traumatic stress disorder (PTSD). Recognizing the unique pressures faced by nurses is the first step towards developing effective strategies to support their psychological well-being.
This article delves into the specific challenges impacting nurses’ mental health and provides essential, actionable self-care tips designed to help nurses navigate the pressures of their profession and safeguard their mental equilibrium. Investing in nurses’ mental health is an investment in the very heart of healthcare.
Understanding the Unique Stressors Impacting Nurses’ Mental Health
To effectively address nurses’ mental health, we must first understand the specific factors contributing to the psychological strain experienced by nurses. These stressors are often multifaceted and interconnected:
- High Workload and Staffing Shortages: Chronic understaffing places immense pressure on existing nurses, leading to heavier patient loads, increased overtime (often mandatory), and rushed care. This constant pressure contributes significantly to stress and burnout, directly impacting nurses’ mental health.
- Emotional Labor: Nurses are expected to manage their own emotions while responding empathetically to the intense emotions of patients and their families. This constant emotional regulation, known as emotional labor, is exhausting and can deplete psychological resources, negatively affecting nurses’ mental health.
- Exposure to Trauma and Suffering: Regularly witnessing pain, critical illness, traumatic injuries, and death takes a significant emotional toll. This vicarious trauma can lead to compassion fatigue and PTSD, serious threats to nurses’ mental health.
- Moral Distress: Nurses often face situations where they know the ethically correct action to take but are constrained by institutional policies, resource limitations, or conflicting demands. This dissonance, known as moral distress, can cause feelings of guilt, anger, and helplessness, undermining nurses’ mental health.
- Shift Work and Long Hours: Disruptions to the natural sleep-wake cycle caused by shift work, combined with extended 12-hour shifts (or longer), lead to physical and mental fatigue. Chronic sleep deprivation is a well-documented risk factor for poor mental health outcomes, making it a crucial consideration for nurses’ mental health. Here’s more about the impacts of night shifts on caregivers’ mental health.
- Workplace Violence and Bullying: Nurses are unfortunately at high risk of experiencing physical and verbal aggression from patients or their families. Additionally, horizontal violence (bullying from colleagues or superiors) can create a toxic work environment, severely damaging morale and nurses’ mental health.
- Lack of Support and Recognition: Feeling undervalued, unsupported by management, or lacking adequate resources can exacerbate feelings of stress and isolation, further compromising nurses’ mental health.
- The Pandemic Effect: The COVID-19 pandemic placed unprecedented strain on healthcare systems and personnel. Nurses faced overwhelming patient surges, critical resource shortages, personal risk of infection, and witnessed immense loss of life, leading to widespread burnout and exacerbating pre-existing issues related to nurses’ mental health.
Understanding these specific pressures highlights the urgent need for proactive strategies focused on preserving and improving nurses’ mental health.
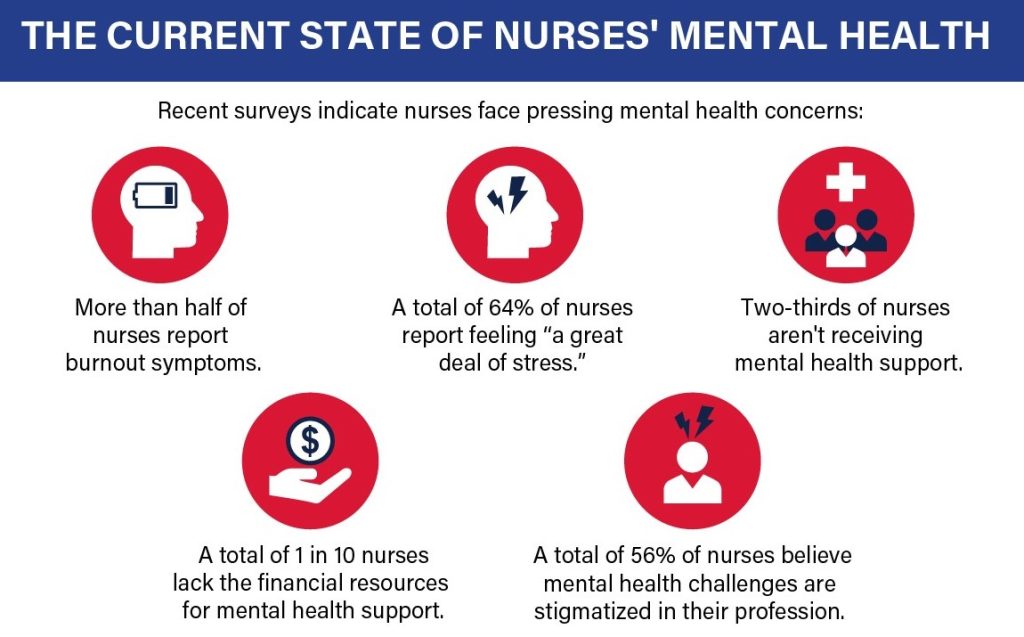
Here is a snapshot of the current state of nurses’ mental health.
Recognizing the Warning Signs: When Nurses’ Mental Health is Compromised
Self-awareness is a cornerstone of maintaining good mental health. Nurses, often focused on the well-being of others, must learn to recognize the signs and symptoms within themselves that indicate their mental health may be suffering. Ignoring these signs can lead to worsening conditions and potentially impair their ability to provide safe care. Key warning signs include:
Emotional Signs:
- Persistent feelings of sadness, hopelessness, or emptiness.
- Increased irritability, frustration, or anger.
- Excessive worry, anxiety, or feeling constantly on edge.
- Feeling emotionally numb or detached (a hallmark of compassion fatigue).
- Loss of interest or pleasure in activities once enjoyed (anhedonia).
- Feelings of guilt, worthlessness, or excessive self-blame.
- Difficulty concentrating or making decisions.
Physical Signs:
- Chronic fatigue, exhaustion, or lack of energy, even after rest.
- Changes in sleep patterns (insomnia, hypersomnia, frequent waking).
- Changes in appetite or weight (significant loss or gain).
- Headaches, muscle tension, or stomach problems with no clear physical cause.
- Increased susceptibility to illness due to a weakened immune system.
Behavioral Signs:
- Withdrawing from social interactions with colleagues, friends, or family.
- Increased use of alcohol, tobacco, or other substances to cope.
- Calling in sick frequently or experiencing presenteeism (being physically present but mentally checked out).
- Making uncharacteristic errors at work.
- Procrastination or difficulty completing tasks.
- Neglecting personal hygiene or appearance.
Recognizing these signs is not a sign of weakness, but rather an important step towards seeking help and implementing self-care strategies to protect nurses’ mental health. Early intervention is key to preventing more severe outcomes.
The Non-Negotiable Nature of Self-Care for Nurses’ Mental Health
Self-care is often mistakenly viewed as a luxury or an indulgence, especially in a profession centered on caring for others. However, for nurses, self-care is not optional; it is a professional and personal necessity. It is the active and intentional process of engaging in activities that promote physical, emotional, and psychological well-being.
Why is self-care so critical for nurses’ mental health?
- Prevents Burnout: Regularly engaging in restorative activities helps replenish depleted energy reserves and buffers against the chronic stress that leads to burnout.
- Enhances Resilience: Self-care practices build emotional and psychological resilience, enabling nurses to better cope with workplace stressors and bounce back from difficult experiences.
- Improves Patient Care: Nurses who prioritize their own well-being are better equipped to provide compassionate, focused, and safe care. Poor nurses’ mental health can correlate with increased medical errors.
- Promotes Longevity in the Profession: Burnout and poor mental health are major drivers of nurses leaving the profession. Self-care can help sustain nurses, reducing turnover rates.
- Models Healthy Behavior: Nurses who practice self-care can serve as positive role models for patients and colleagues, promoting a broader culture of well-being.
Making self-care a non-negotiable part of their routine is one of the most powerful actions nurses can take to safeguard their nurses’ mental health.

Essential Self-Care Strategies for Nurses
Effective self-care is personalized, but certain strategies are particularly beneficial for addressing the unique challenges faced by nurses. Integrating these practices into daily life can significantly bolster nurses’ mental health.
1. Prioritize Physical Foundations:
The mind and body are inextricably linked. Neglecting physical health inevitably impacts mental health.
- Optimize Sleep: Aim for 7-9 hours of quality sleep per night. This is challenging with shift work, but strategies like maintaining a consistent sleep schedule (even on days off), creating a dark and quiet sleep environment, avoiding caffeine and heavy meals before bed, and using blackout curtains can help. Protect sleep fiercely; it’s fundamental to nurses’ mental health.
- Nourish Your Body: Fueling your body with nutritious food provides sustained energy and supports brain function. Pack healthy meals and snacks for shifts, stay hydrated by drinking plenty of water, and limit processed foods, excessive sugar, and caffeine. Good nutrition supports good nurses’ mental health.
- Move Your Body: Regular physical activity is a powerful stress reliever and mood booster. Find activities you enjoy, whether it’s walking, running, swimming, dancing, yoga, or team sports. Even short bursts of activity during breaks (like stretching or a quick walk) can make a difference. Exercise is a proven intervention for improving nurses’ mental health.
2. Cultivate Emotional and Psychological Well-being:
Actively tending to emotional needs is crucial for navigating the psychological demands of nursing.
- Practice Mindfulness and Meditation: Mindfulness involves paying attention to the present moment without judgment. Techniques like deep breathing exercises, body scans, or short guided meditations can be practiced even during busy shifts to reduce acute stress. Regular practice builds resilience and improves emotional regulation, benefiting nurses’ mental health. Apps like Calm, Headspace, or Insight Timer offer accessible resources.
- Set Healthy Boundaries: Learn to say no to extra shifts or responsibilities when you are already feeling overwhelmed. Protect your days off by consciously disconnecting from work – avoid checking emails or constantly talking about work. Establishing clear boundaries between work and personal life is vital for preserving nurses’ mental health.
- Acknowledge and Process Emotions: Don’t suppress difficult feelings. Find healthy ways to process the emotional weight of nursing. This could involve:
- Journaling: Writing down thoughts and feelings can provide clarity and emotional release.
- Debriefing: Talking about challenging experiences with trusted colleagues or mentors who understand the context can be incredibly validating and helpful. Formal debriefing sessions after critical incidents are also important.
- Creative Expression: Engaging in art, music, or other creative outlets can be a therapeutic way to process emotions.
- Engage in Meaningful Hobbies: Make time for activities outside of nursing that bring you joy, relaxation, or a sense of accomplishment. Hobbies provide a necessary mental break and help maintain a sense of identity beyond being “a nurse.” This detachment is important for nurses’ mental health.
3. Leverage Social Support Systems:
Connection is a powerful buffer against stress and isolation.
- Connect with Peers: Build supportive relationships with colleagues. Sharing experiences, offering mutual support, and validating each other’s struggles can significantly alleviate feelings of isolation and stress. Peer support programs can be invaluable for nurses’ mental health.
- Nurture Personal Relationships: Invest time and energy in relationships with friends and family outside of work. These connections provide perspective, emotional support, and a reminder of life beyond the hospital walls. Explain the demands of your job so they can better understand and support your needs related to nurses’ mental health.
- Seek Professional Help: There is no shame in seeking support from a mental health professional (therapist, counselor, psychologist). Therapy provides a confidential space to process experiences, learn coping strategies, and address underlying mental health conditions. Many employee assistance programs (EAPs) offer free or subsidized counseling sessions. Normalizing seeking help is crucial for improving nurses’ mental health across the profession.
4. Implement Workplace Strategies:
Self-care also involves strategies employed during the workday itself.
- Utilize Breaks Effectively: Don’t skip breaks, even when busy. Use this time to truly disconnect: step away from the unit, get fresh air, hydrate, eat mindfully, or practice a quick relaxation technique. Even micro-breaks (a minute of deep breathing) can help reset the nervous system. Protecting break times supports nurses’ mental health.
- Practice Self-Compassion: Be kind to yourself, especially after difficult shifts or perceived mistakes. Acknowledge that nursing is incredibly challenging, and you are doing your best in often difficult circumstances. Replace self-criticism with self-compassion to protect your nurses’ mental health.
- Seek Mentorship and Supervision: Engaging with experienced mentors or participating in clinical supervision can provide guidance, support, and opportunities for reflection, which are beneficial for navigating professional challenges and maintaining nurses’ mental health.
- Advocate for Change: While individual self-care is vital, systemic issues also need addressing. Advocate for safer staffing levels, better resources, policies against workplace violence, and a culture that genuinely supports nurses’ mental health. Collective action can create a healthier work environment for everyone.
Overcoming Barriers to Self-Care
Nurses often face significant barriers to implementing self-care practices:
- Time Constraints: Long hours and demanding schedules leave little perceived time or energy for self-care. Solution: Start small. Even 5-10 minutes of mindfulness or stretching can help. Schedule self-care like any other important appointment.
- Guilt: Nurses may feel guilty taking time for themselves when others need care. Solution: Reframe self-care as essential for providing good care. You cannot pour from an empty cup. Prioritizing your well-being enables you to be a better nurse.
- Stigma: Fear of judgment or negative career consequences can prevent nurses from acknowledging struggles or seeking help for nurses’ mental health issues. Solution: Promote open conversations about mental health, share personal experiences (if comfortable), and advocate for destigmatizing mental health support in the workplace.
- Lack of Resources or Knowledge: Some nurses may not know where to start or lack access to resources. Solution: Utilize EAPs, explore free online resources (apps, articles, podcasts), connect with supportive colleagues, and advocate for workplace wellness programs.
Acknowledging these barriers is the first step to finding creative solutions and making self-care a sustainable practice for improving nurses’ mental health.

The Crucial Role of Healthcare Organizations in Supporting Nurses’ Mental Health
While individual self-care is paramount, the responsibility for nurses’ mental health does not rest solely on the individual nurse. Healthcare organizations have a profound ethical and operational obligation to create work environments that actively support and protect the mental well-being of their staff. Systemic changes are needed to address the root causes of stress and burnout.
Organizational responsibilities include:
- Ensuring Safe Staffing Levels: Adequate staffing is arguably the single most impactful factor in reducing workload stress and improving both patient safety and nurses’ mental health.
- Promoting a Culture of Respect and Safety: Implementing zero-tolerance policies for workplace violence and bullying, and fostering a culture where nurses feel psychologically safe to speak up and support one another.
- Providing Accessible Mental Health Resources: Offering robust EAPs, confidential counseling services, peer support programs, and mental health days. Making these resources well-known and easy to access is key.
- Supporting Work-Life Balance: Implementing fair scheduling practices, respecting days off, and discouraging a culture of constant availability.
- Training Leadership: Equipping nurse managers and leaders with the skills to recognize signs of distress, offer support, and foster a mentally healthy team environment. Their role in championing nurses’ mental health is vital.
- Facilitating Debriefing and Support: Providing structured opportunities for debriefing after critical incidents or traumatic events.
- Investing in Wellness Programs: Offering resources and initiatives focused on stress management, resilience building, physical fitness, and overall nurses’ mental wellbeing.
A true commitment to nurses’ mental health requires a partnership between individual nurses practicing self-care and healthcare organizations creating supportive systems.
Research and Continued Learning
The field of nurses’ mental health is an area of ongoing research and critical importance. Understanding the nuances of compassion fatigue, burnout, moral injury, and effective interventions requires continuous study. For students or researchers exploring this vital topic, seeking help with a research paper about nurses’ mental health from academic advisors, library resources, and reputable databases (like PubMed, CINAHL) is encouraged.
In case you need help with writing research papers, term papers, TEAS exams, assignments, essays, case studies, thesis or even dissertations on nurses’ mental health, do not hesitate to engage Nursing Papers. We offer professional academic writing services that cover topic suggestion, paper writing, proofreading, editing, formatting and plagiarism removal.
Staying informed about the latest findings and best practices benefits individual nurses and the profession as a whole. The focus must remain on improving not just coping mechanisms but also the fundamental conditions that impact nurses’ mental health.
Conclusion: A Call to Prioritize Nurses’ Mental Health
Nurses are the backbone of our healthcare system, providing essential care with skill, compassion, and dedication. However, the immense pressures of the profession place their psychological well-being at significant risk. Prioritizing nurses’ mental health is not merely an act of kindness; it is a strategic imperative for retaining skilled professionals, ensuring patient safety, and sustaining the health of our communities.
Self-care is a critical toolset that empowers nurses to navigate the emotional and physical demands of their work. By integrating practices that support physical health, emotional processing, social connection, and workplace well-being, nurses can build resilience and protect their mental health. However, individual efforts must be matched by organizational commitment to creating healthier, safer, and more supportive work environments.
Let this be a call to action for individual nurses to embrace self-care without guilt, for colleagues to support one another, and for healthcare leaders to champion systemic changes that genuinely value and protect nurses’ mental health. Caring for the carers is essential, ensuring that those who dedicate their lives to healing others are themselves healthy, supported, and whole. The future of nursing, and indeed healthcare, depends on our collective commitment to nurturing nurses’ mental health. It’s time we make nurses’ mental health an undeniable priority.