Table of Contents
Introduction: The Imperative of Culturally Competent Care
The landscape of healthcare is increasingly diverse. Patients entering hospitals, clinics, and community health settings come from a vast array of cultural, ethnic, linguistic, and religious backgrounds. This rich tapestry presents both opportunities and challenges for healthcare providers, particularly nurses, who are often at the forefront of patient interaction and care delivery. In this context, nursing and cultural competence is not merely a desirable skill; it is an absolute necessity for providing safe, effective, ethical, and patient-centered care.
This guide provides a comprehensive overview of nursing and cultural competence, exploring its definition, importance, components, practical strategies, challenges, and its evolution towards concepts like cultural humility and safety. Understanding and implementing the principles of nursing and cultural competence is fundamental to bridging health disparities and improving outcomes for all patient populations. The journey towards achieving meaningful nursing and cultural competence requires ongoing learning, reflection, and a genuine commitment from individual nurses and the healthcare systems they work within. This exploration underscores why mastering nursing and cultural competence is critical for the modern nursing profession.
What is Culture? Laying the Groundwork
Before delving into cultural competence, it’s essential to understand the concept of ‘culture’ itself. Culture is often defined as the learned, shared, and transmitted values, beliefs, norms, and lifeway practices of a particular group that guide thinking, decisions, and actions in patterned ways. It encompasses far more than just ethnicity or nationality.
Key aspects of culture include:
- Shared Beliefs and Values: Underlying principles that guide behaviour and worldview (e.g., beliefs about health, illness, healing, family roles, respect for authority).
- Communication Patterns: Verbal language, tone, non-verbal cues (eye contact, personal space, gestures), and communication styles (direct vs. indirect).
- Social Structures: Family organization, community dynamics, gender roles, and social hierarchies.
- Dietary Practices: Food preferences, restrictions, rituals around food.
- Religious and Spiritual Beliefs: Practices, rituals, beliefs about life, death, suffering, and healing.
- Health Beliefs and Practices: Perceptions of illness causality, traditional healing methods, attitudes towards Western medicine, pain expression, and end-of-life care preferences.
- Time Orientation: Emphasis on past, present, or future, which can influence appointment keeping and adherence to long-term treatment plans.
It is crucial to recognize that culture is:
- Dynamic: It changes over time and with exposure to other cultures.
- Heterogeneous: Not everyone within a cultural group thinks or behaves identically. Avoid stereotyping.
- Individualized: Each person’s experience of their culture is unique, influenced by factors like age, gender, socioeconomic status, education, sexual orientation, and level of acculturation.
Understanding these facets of culture provides the foundation upon which effective nursing and cultural competence is built.
Defining Cultural Competence in Nursing
Cultural competence in nursing refers to the ability of nurses to understand, appreciate, and effectively work with individuals from cultures different from their own. It involves developing an awareness of one’s own cultural biases, acquiring knowledge of diverse cultural practices and worldviews, and mastering skills to provide culturally appropriate care. It’s a complex integration of knowledge, attitudes, and skills that enhances cross-cultural communication and enables the delivery of care that respects patients’ values and needs.
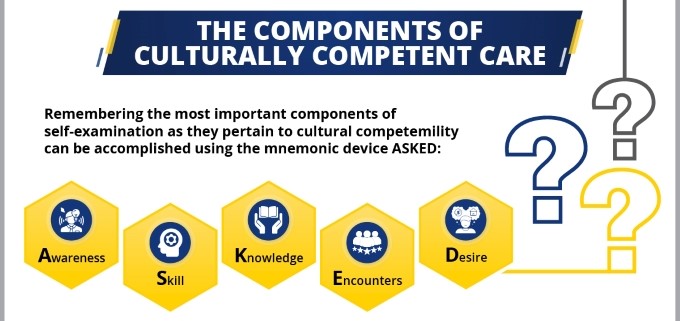
Several models conceptualize nursing and cultural competence. One widely recognized framework is Dr. Josepha Campinha-Bacote’s “The Process of Cultural Competence in the Delivery of Healthcare Services.” This model views cultural competence as an ongoing process, not an endpoint, and comprises five interrelated constructs:
- Cultural Awareness: The process of self-examination and in-depth exploration of one’s own cultural and professional background, including recognizing personal biases, prejudices, and assumptions about individuals who are different.
- Cultural Knowledge: Seeking and obtaining a sound educational foundation concerning diverse cultural and ethnic groups. This involves understanding their worldviews, health-related beliefs, disease incidence/prevalence, and treatment efficacy.
- Cultural Skill: The ability to collect relevant cultural data regarding the patient’s presenting problem and accurately perform a culturally specific assessment. This requires knowing how to use appropriate communication and assessment tools.
- Cultural Encounters: Directly engaging in face-to-face interactions with patients from culturally diverse backgrounds to refine or modify existing beliefs about a cultural group and prevent stereotyping.
- Cultural Desire: The motivation of the nurse to want to engage in the process of becoming culturally aware, knowledgeable, skillful, and familiar with cultural encounters. This is seen as the pivotal “pivot” of the model – it must stem from genuine aspiration, not just obligation.
Achieving genuine nursing and cultural competence is a developmental journey requiring commitment and continuous effort. It moves beyond tolerance to embrace and respond effectively to cultural differences.
Why is Nursing and Cultural Competence Crucial?
The integration of nursing and cultural competence into practice is not optional; it is central to achieving core healthcare goals. Its importance is multifaceted:
- Addressing Health Disparities: Significant disparities in health outcomes exist among different racial, ethnic, and cultural groups. These disparities are often linked to barriers in accessing care, communication breakdowns, and implicit bias within the healthcare system. A lack of nursing and cultural competence can perpetuate these inequalities. Conversely, culturally competent care can help mitigate these disparities by tailoring care to meet specific needs.
- Improving Patient Safety: Misunderstandings arising from cultural or linguistic differences can lead to serious medical errors. This includes incorrect diagnoses, medication errors (due to misunderstood instructions), lack of informed consent, and adverse events. Strong nursing and cultural competence enhances communication clarity, ensuring patients understand their conditions and treatments, thereby reducing the risk of errors.
- Enhancing Patient Trust and Communication: Patients are more likely to trust and communicate openly with healthcare providers who demonstrate respect for their cultural background, beliefs, and values. Effective nursing and cultural competence builds rapport, fostering a therapeutic relationship where patients feel comfortable sharing vital health information and asking questions.
- Increasing Treatment Adherence: When care plans conflict with a patient’s cultural beliefs, values, or lifestyle, adherence is likely to be poor. Culturally competent nurses work collaboratively with patients to develop treatment plans that are not only clinically sound but also culturally acceptable and feasible. This collaborative approach, rooted in nursing and cultural competence, significantly improves adherence.
- Promoting Patient Satisfaction: Patients who feel their cultural needs are understood and respected report higher levels of satisfaction with their care. Feeling heard, valued, and treated with dignity contributes positively to the overall patient experience. Excellent nursing and cultural competence directly contributes to this positive experience.
- Meeting Ethical and Professional Standards: Major nursing organizations, like the American Nurses Association (ANA), emphasize the ethical obligation of nurses to provide culturally congruent care. The ANA Code of Ethics for Nurses requires nurses to practice with compassion and respect for the inherent dignity, worth, and unique attributes of every person. Fulfilling this mandate requires a deep commitment to nursing and cultural competence. It is, therefore, an ethical imperative.
Key Components and Strategies for Nursing and Cultural Competence
Building nursing and cultural competence is an active and ongoing process. It involves developing specific attitudes, knowledge bases, and skills. Here are key components and practical strategies:
1. Cultivating Cultural Awareness:
- Self-Reflection: Regularly examine your own cultural background, values, beliefs, biases, and assumptions. How might these influence your interactions with patients from different backgrounds? Journaling about challenging cross-cultural encounters can be insightful.
- Identifying Biases: Acknowledge that everyone holds implicit biases. The goal is not to be bias-free (which is arguably impossible) but to recognize biases and consciously work to prevent them from affecting patient care. Tools like the Implicit Association Test (IAT) can help uncover unconscious biases. This awareness is the cornerstone of nursing and cultural competence.
2. Acquiring Cultural Knowledge:
- Learn About Common Cultures: Familiarize yourself with the predominant cultural groups within your service area. Focus on their health beliefs, communication styles, family structures, dietary practices, and religious beliefs relevant to healthcare.
- Utilize Reputable Resources: Consult academic literature, cultural health websites (e.g., EthnoMed), community organizations, and diversity/inclusion training materials.
- Ask Patients Respectfully: Recognize that the patient is the expert on their own culture and preferences. Ask open-ended questions about what is important to them regarding their care. Acquiring knowledge is vital for effective nursing and cultural competence.
3. Honing Cultural Skill:
- Culturally Sensitive Communication:
- Use Professional Interpreters: Rely on qualified medical interpreters, not family members (especially children), for language barriers. Speak directly to the patient, not the interpreter. Use short sentences and avoid jargon.
- Non-Verbal Communication: Be mindful of eye contact, personal space, touch, and gestures, as their meanings vary significantly across cultures. Ask about preferences if unsure.
- Plain Language: Avoid medical jargon and use clear, simple language.
- Teach-Back Method: Ask patients to explain information back in their own words to ensure understanding.
- Cultural Assessment:
- Integrate cultural assessment into your routine nursing assessment. Ask questions about health beliefs, traditional practices, dietary needs, spiritual resources, and family involvement.
- Use assessment tools like the LEARN model (Listen, Explain, Acknowledge, Recommend, Negotiate) to guide conversations about treatment plans. Applying these skills demonstrates practical nursing and cultural competence.
4. Seeking Cultural Encounters:
- Engage Intentionally: Seek opportunities to interact with people from diverse backgrounds, both within and outside the workplace. Attend cultural events, volunteer in diverse communities, and engage in dialogue.
- Learn from Interactions: View each cross-cultural encounter as a learning opportunity. Reflect on what went well and what could be improved. Direct experience significantly builds nursing and cultural competence.
5. Nurturing Cultural Desire:
- Embrace Humility: Recognize that you don’t know everything about other cultures and approach interactions with a spirit of learning and humility.
- Commit to Lifelong Learning: View cultural competence as an ongoing journey, not a destination. Actively seek out continuing education, workshops, and resources related to nursing and cultural competence.
- Advocate for Patients: Use your understanding to advocate for culturally appropriate care for your patients within the healthcare system. This intrinsic motivation fuels the continuous development of nursing and cultural competence.

Practical Strategies for Nurses in Daily Practice
- Initial Interaction: Greet patients respectfully, using their preferred name and title. Ask how they would like to be addressed.
- Assessment: Use open-ended questions: “What do you think caused your illness?” “What worries you most about this?” “Are there any traditional remedies you use?” “How does your family usually handle health decisions?”
- Care Planning: Involve the patient and family (as appropriate) in developing the care plan. Acknowledge and, where safe and feasible, integrate cultural preferences (e.g., dietary needs, prayer times, family presence).
- Communication: Always verify understanding. Be patient and allow extra time for communication, especially when using interpreters.
- Dietary Needs: Assess for religious or cultural dietary restrictions or preferences. Collaborate with dietary services to accommodate these needs.
- Spiritual Care: Inquire about spiritual or religious practices that are important to the patient, especially during times of stress or end-of-life care. Facilitate access to spiritual advisors if requested.
- End-of-Life Care: Discuss preferences regarding death rituals, autopsy, organ donation, and family involvement sensitively, recognizing cultural variations. Strong nursing and cultural competence is particularly vital in these sensitive situations.
Challenges and Barriers to Nursing and Cultural Competence
Despite its importance, achieving widespread nursing and cultural competence faces several hurdles:
- Stereotyping vs. Generalizing: It’s easy to fall into the trap of stereotyping (applying assumptions about a group to an individual without verification) rather than generalizing (using cultural knowledge as a starting point for inquiry). Cultural competence requires individualizing care.
- Time Constraints: Busy clinical environments often limit the time available for in-depth cultural assessments and communication.
- Lack of Resources: Insufficient access to qualified interpreters, translated materials, and culturally appropriate resources can hinder efforts.
- Implicit Bias: Unconscious biases held by healthcare providers can negatively impact interactions and care decisions, even among those who consciously value equality.
- Institutional Barriers: Lack of organizational commitment, inadequate training, policies that aren’t culturally sensitive, and a non-diverse workforce can create systemic barriers.
- Complexity of Culture: The multifaceted and dynamic nature of culture makes it impossible to be an expert on every culture. The focus should be on developing the skills to navigate diversity effectively.
- Language Barriers: Communication is foundational, and language differences pose a significant challenge that requires specific resources (interpreters) to overcome.
Overcoming these challenges requires a concerted effort from individual nurses, educators, researchers, and healthcare organizations committed to fostering nursing and cultural competence.
Moving Beyond Competence: Cultural Humility and Cultural Safety
While nursing and cultural competence provides a crucial foundation, contemporary discourse increasingly emphasizes the concepts of cultural humility and cultural safety.
- Cultural Humility: Introduced by Tervalon and Murray-García (1998), cultural humility involves a lifelong commitment to self-evaluation and self-critique, redressing power imbalances in the patient-provider relationship, and developing mutually beneficial partnerships with communities on behalf of individuals and defined populations. It emphasizes humility, acknowledging that the patient is the expert on their own experience, rather than the provider achieving a state of “competence.”
- Cultural Safety: Originating from the work of Irihapeti Ramsden with Māori nurses in New Zealand, cultural safety focuses on the patient’s experience. It is defined as an environment where the patient feels safe, respected, and culturally secure – meaning there is no assault, challenge, or denial of their identity, who they are, and what they need. The determination of whether care is culturally safe rests with the patient, not the provider.
These concepts are not replacements for nursing and cultural competence but rather represent an evolution and deepening of its principles. They shift the focus from the provider’s knowledge acquisition (competence) to the provider’s ongoing self-reflection and attitude (humility) and the patient’s subjective experience of care (safety). Excellent nursing and cultural competence should ideally lead to practices embodying cultural humility and resulting in culturally safe care environments.
Education and Research in Nursing and Cultural Competence
Education and research are vital for advancing nursing and cultural competence within the profession.
- Nursing Curricula: Nursing programs must integrate comprehensive education on nursing and cultural competence throughout the curriculum, not just as a single module. This should include theory, simulated experiences, and clinical practice opportunities in diverse settings. Students need foundational knowledge and skills practice.
- Continuing Professional Development: Cultural competence is not static. Hospitals, healthcare systems, and professional organizations must provide ongoing training and resources for practicing nurses to continually update their knowledge and skills related to nursing and cultural competence.
- Research: Further research is needed to understand the most effective strategies for teaching and implementing nursing and cultural competence, its impact on patient outcomes, and how to best address systemic barriers. Students and researchers often require help with research paper about nursing and cultural competence from Nursing Papers to explore these complex issues, contributing valuable insights to the field.
Advanced scholarly work, such as completing a nursing and cultural competence dissertation, plays a critical role in generating new knowledge and evidence-based practices. Robust research underpins the continuous improvement of nursing and cultural competence. Besides research papers and dissertations, we can also help you with writing essays, term papers, assignments, case studies and thesis about nursing and cultural competence.

Organizational Responsibility: Creating Culturally Competent Systems
While individual nurses bear responsibility for developing their own cultural competence, healthcare organizations play a critical role in creating an environment where culturally competent care can flourish. Organizational responsibilities include:
- Leadership Commitment: Leaders must champion diversity, equity, and inclusion, making nursing and cultural competence a strategic priority.
- Policies and Procedures: Implement policies that support culturally competent care, such as mandatory interpreter services, collection of patient demographic data (including language and ethnicity), and culturally sensitive care protocols.
- Workforce Diversity: Recruit, retain, and promote a diverse nursing workforce that reflects the patient population served.
- Training and Education: Provide comprehensive and ongoing training on nursing and cultural competence for all staff.
- Resource Allocation: Ensure adequate resources are available, including professional interpreters, translated materials, and community health workers or patient navigators.
- Community Engagement: Partner with local communities to understand their health needs and cultural perspectives, ensuring services are relevant and accessible.
- Data Collection and Quality Improvement: Collect data on patient experiences and outcomes stratified by race, ethnicity, and language. Use this data to identify disparities and drive quality improvement initiatives focused on enhancing nursing and cultural competence. Systemic support is absolutely essential for achieving widespread and sustainable nursing and cultural competence.
Conclusion: The Ongoing Journey Towards Equitable Care
Nursing and cultural competence is far more than a buzzword; it is the bedrock of equitable, high-quality nursing care in our increasingly diverse world. It requires nurses to engage in a continuous process of self-reflection, knowledge acquisition, skill development, and intentional engagement with diverse patient populations. The journey involves moving beyond mere awareness to actively integrating cultural understanding into every aspect of patient assessment, communication, and care planning.
The benefits are profound: reduced health disparities, improved patient safety, enhanced trust, better treatment adherence, and greater patient satisfaction. While challenges exist, including time constraints, resource limitations, and implicit biases, they can be overcome through dedicated individual effort and robust organizational support. Embracing concepts like cultural humility and striving for cultural safety further deepens the commitment to patient-centered care, ensuring that patients not only receive clinically effective treatment but also feel respected, understood, and safe within the healthcare system.
Ultimately, the commitment to nursing and cultural competence reflects the core values of the nursing profession – compassion, respect for human dignity, and advocacy for all patients. It is an ongoing journey, demanding dedication, humility, and a persistent desire to learn and grow. By championing and practicing nursing and cultural competence, nurses can make a significant difference in the lives of their patients and contribute to a more just and equitable healthcare system for everyone. The future of excellent nursing care hinges on our collective ability to master and embody nursing and cultural competence.