Table of Contents
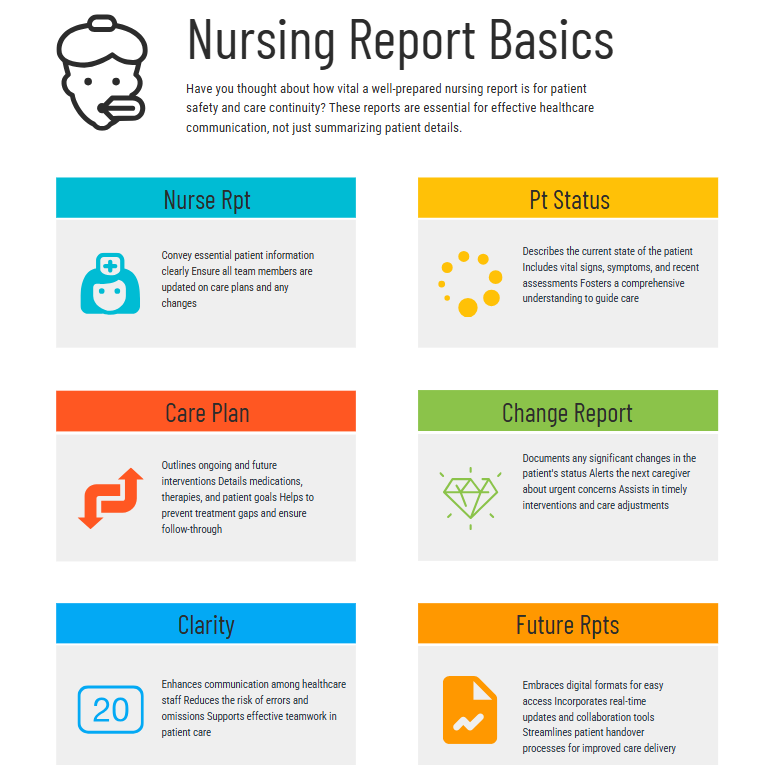
The nursing report, a cornerstone of effective patient care, is far more than a simple recounting of events. It’s a dynamic communication tool that ensures continuity of care, promotes patient safety, and facilitates collaboration amongst the healthcare team. A well-written nursing report is concise, accurate, and comprehensive, providing all the necessary information for the incoming nurse to seamlessly continue providing high-quality care.
This article will discuss the intricacies of crafting a superior nursing report, covering everything from structure and content to best practices and common pitfalls to avoid. Mastering the art of the nursing report is crucial for any nurse, and this guide will empower you to become proficient in this vital aspect of your profession.
Understanding the Purpose of the Nursing Report
The primary purpose of the nursing report is to provide a clear and concise handover of patient information. This ensures that the incoming nurse is fully informed about the patient’s condition, treatment plan, and any recent changes or concerns. The effectiveness of the report directly impacts the quality and safety of patient care. A poorly written or incomplete nursing report can lead to medication errors, missed diagnoses, and potentially harmful delays in treatment. Conversely, a well-structured and informative nursing report enables a smooth transition of care, minimizing disruptions and maximizing patient well-being. In essence, the nursing report is a vital link in the chain of patient care, ensuring the continuity and quality of services.
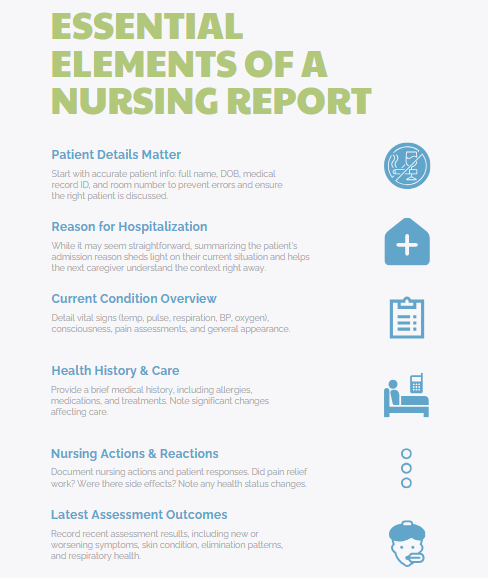
Structuring Your Nursing Report: A Step-by-Step Guide
While the specific format may vary between institutions, most effective nursing reports follow a similar structure. Consistency in format is crucial for clarity and efficiency. Here’s a suggested structure for comprehensive nursing reports:
- Patient Identification: Begin by clearly stating the patient’s name, date of birth, medical record number, and room number. This seemingly simple step is crucial to prevent errors and ensure you are discussing the correct patient. Any misidentification can have serious consequences.
- Reason for Admission: Briefly summarize the reason the patient was admitted to the hospital or facility. This provides immediate context for the incoming nurse.
- Current Status: This section forms the core of the report and should be the most detailed. Describe the patient’s current condition, including vital signs (temperature, pulse, respiration, blood pressure, oxygen saturation), level of consciousness, pain level (using a standardized pain scale), and overall appearance.
- Medical History and Treatment: Briefly summarize the patient’s relevant medical history, including any significant allergies, current medications, and ongoing treatments. This section should highlight any recent changes or significant events related to their medical management. If a patient has recently undergone a procedure or surgery, detail that as well. The report should accurately and comprehensively reflect the patient’s journey.
- Nursing Interventions and Responses: Detail the nursing interventions performed and the patient’s response to those interventions. For example, did the patient respond well to pain medication? Did they exhibit any adverse reactions to medications? Note any changes in the patient’s condition that were directly related to nursing interventions.
- Assessment Findings: Document your most recent assessment findings, including any new or worsening symptoms. This section might include observations of skin integrity, bowel and bladder function, respiratory status, and any other relevant observations.
- Plan of Care: Outline the plan of care for the upcoming shift, including any planned interventions, medications, or tests. This section serves as a roadmap for the incoming nurse, indicating the immediate priorities and planned actions. A comprehensive report aids in seamless transition and continuity of treatment.
- Outstanding Issues or Concerns: Highlight any unresolved issues or concerns that require immediate attention. This could include pending lab results, worsening symptoms, or patient anxieties. This section ensures that critical matters are promptly addressed.
- Significant Events: If any significant events occurred during your shift (falls, changes in mental status, allergic reactions, etc.), these must be documented thoroughly and accurately in the nursing report. This information is critical for patient safety.
Best Practices for Effective Nursing Reports
- Use Clear and Concise Language: Avoid medical jargon and use plain language that is easily understood by all members of the healthcare team.
- Be Accurate and Objective: Stick to the facts and avoid personal opinions or interpretations. Document only what you have observed or verified.
- Maintain Confidentiality: Always protect patient confidentiality by avoiding the use of identifying information in informal settings.
- Document Thoroughly: Don’t leave out any important details, no matter how seemingly insignificant. Complete documentation is critical for continuity of care. Omitting crucial information in the nursing report can compromise patient safety.
- Use Standardized Terminology: Utilizing standardized terminology ensures consistency and clarity across all nursing reports.
- Timeliness: Complete the report promptly and accurately at the end of your shift to ensure a smooth transition. Delays can compromise the efficiency of care. A timely nursing report is a hallmark of professional practice.
The Nursing Report and Teamwork
Effective communication is essential in healthcare. The report facilitates this by ensuring that all members of the healthcare team are informed and working from the same information base. It fosters collaboration, promoting efficient and effective patient care. The quality of the report significantly impacts the effectiveness of teamwork. A thorough and accurate report allows for collaborative decision-making and improved patient outcomes.
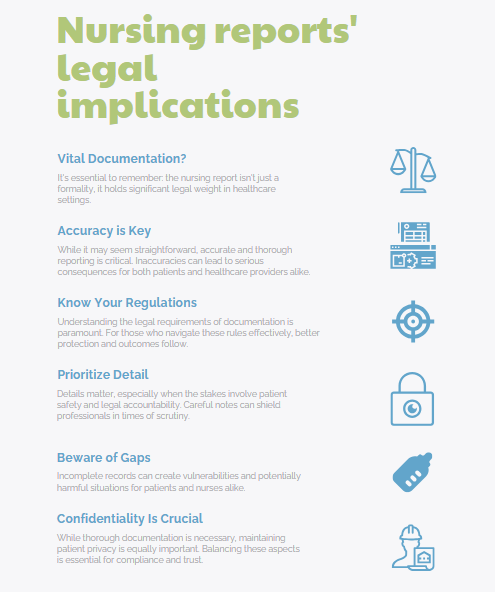
The Legal Implications of the Nursing Report
The nursing report serves as a legal document. Accurate and complete documentation protects both the patient and the nurse. It serves as evidence of the care provided and can be used in legal proceedings if necessary. Therefore, maintaining meticulous accuracy is crucial. An incomplete or inaccurate report can have significant legal implications.
The Common Mistakes to Avoid in a Nursing Report
Effective communication is the bedrock of safe and efficient patient care, and the nursing report is the crucial bridge connecting shifts and care providers. A poorly executed report, however, can lead to errors, delays in treatment, and even compromise patient safety. Avoiding common pitfalls is essential for delivering high-quality care and ensuring a smooth transition between shifts. This article highlights some frequent mistakes to avoid in your next nursing report.
Vague or Incomplete Information
Rushing through the report to catch a break or attend to other pressing tasks is a recipe for disaster. A thorough report should cover all essential aspects of the patient’s condition, including their vital signs, medications administered, treatments received, response to interventions, and any significant changes in their status. Omitting key information can leave the oncoming nurse unprepared and potentially lead to misjudgments or delayed care.
For instance, failing to mention a patient’s allergy to a specific medication could have serious consequences. Similarly, neglecting to document a recent fall or a sudden change in mental status could delay appropriate intervention. A comprehensive nursing report acts as a safety net, providing the receiving nurse with a complete picture of the patient’s current needs and care plan.
Lack of clarity and conciseness
Using vague language or medical jargon without explanation can be confusing and lead to misinterpretations. Instead of saying “patient is doing poorly,” specify the observable signs and symptoms: “Patient is exhibiting increased shortness of breath, decreased oxygen saturation, and reports chest pain.” Using precise language, quantifiable data (e.g., specific blood pressure readings, oxygen saturation levels), and avoiding medical abbreviations unless universally understood within the healthcare facility promotes clear and accurate communication. Remember, the goal of nursing reports is to ensure continuity of care, not to impress with medical terminology.
Poor Organization
Poor organization is yet another frequent issue. Jumping haphazardly between different aspects of the patient’s condition makes the report difficult to follow and increases the likelihood of important details being missed. A structured approach, following a consistent format (e.g., head-to-toe assessment, systems approach), ensures that all relevant information is covered systematically. Many hospitals have standardized reporting forms or templates to promote consistency, and using these aids can significantly improve organization and prevent omissions. Consider prioritizing information, addressing the most urgent or critical needs first. For instance, if a patient has experienced a significant change in their condition, that should be the focus of the initial part of the report.
Missing Information
Neglecting to document the patient’s response to treatment is a significant oversight. A complete nursing report should outline not only what treatments were administered but also how the patient responded to them. Did the pain medication provide relief? Did the oxygen therapy improve their oxygen saturation? Documenting the effectiveness (or lack thereof) of interventions allows the oncoming nurse to adjust the care plan appropriately and continue providing optimal care.
Inaccurate or Unverifiable Information
Finally, relying solely on written or verbal nursing reports without facilitating a direct handover can compromise effective communication. While a detailed written report is crucial, a brief face-to-face interaction allows for clarification of specific concerns, addressing immediate needs, and allows for a more complete understanding of the patient’s overall condition. This provides an opportunity for the nurses to ask questions, discuss any uncertainties, and ensure a smooth transition of care. A comprehensive approach that combines a well-structured written report with a verbal handover is essential for optimal patient safety.
In conclusion, a meticulously prepared nursing report is not just a bureaucratic requirement, but a vital component of safe and effective patient care. By avoiding these common mistakes, nurses can significantly improve communication, ensure continuity of care, and ultimately enhance the quality of care delivered to their patients. A well-executed nursing report is a testament to the professional commitment of every nurse involved in the patient’s care journey.
Frequently Asked Questions about Nursing Reports
The nursing report, that crucial handover between shifts, is often the subject of much discussion and, let’s face it, occasional anxiety. Whether you’re a seasoned nurse or a fresh graduate, understanding the intricacies of a well-executed nursing report is paramount for patient safety and efficient care. The following are some of the most frequently asked questions surrounding this vital aspect of nursing practice.
What exactly is a nursing report, and why is it so important?
A nursing report is a structured communication process where nurses exchange vital information about their patients. It’s not just a recitation of facts; it’s a dynamic exchange designed to ensure continuity of care, prevent medical errors, and facilitate collaborative decision-making. The effectiveness of a nursing report directly impacts patient outcomes, contributing to improved safety and reduced risks. A thorough report minimizes the potential for missed diagnoses, medication errors, or delayed treatment, thus ensuring a smooth transition between shifts and consistent, high-quality care. A poorly executed nursing report, on the other hand, can lead to fragmented care, miscommunication, and potentially dangerous situations.
What information should be included in a comprehensive nursing report?
A comprehensive nursing report typically includes the following key elements:
- Patient demographics: Name, age, date of birth, medical record number.
- Reason for admission: Briefly state the primary diagnosis and relevant medical history.
- Current medical status: Include vital signs (temperature, heart rate, blood pressure, respiratory rate, oxygen saturation), level of consciousness, pain assessment, and any recent changes in the patient’s condition.
- Treatment plan: Outline the current medications, treatments (e.g., oxygen therapy, intravenous fluids), and any planned procedures or tests.
- Nursing interventions: Detail any significant nursing actions performed, including wound care, medication administration, and patient education.
- Outstanding issues: Highlight any unresolved problems or concerns requiring immediate attention, such as pending lab results, consultations with specialists, or potential complications.
- Patient’s response to treatment: Describe the patient’s response to current interventions, noting any positive or negative changes.
- Family/significant other involvement: Mention any relevant information about the patient’s support system and their level of involvement in care.
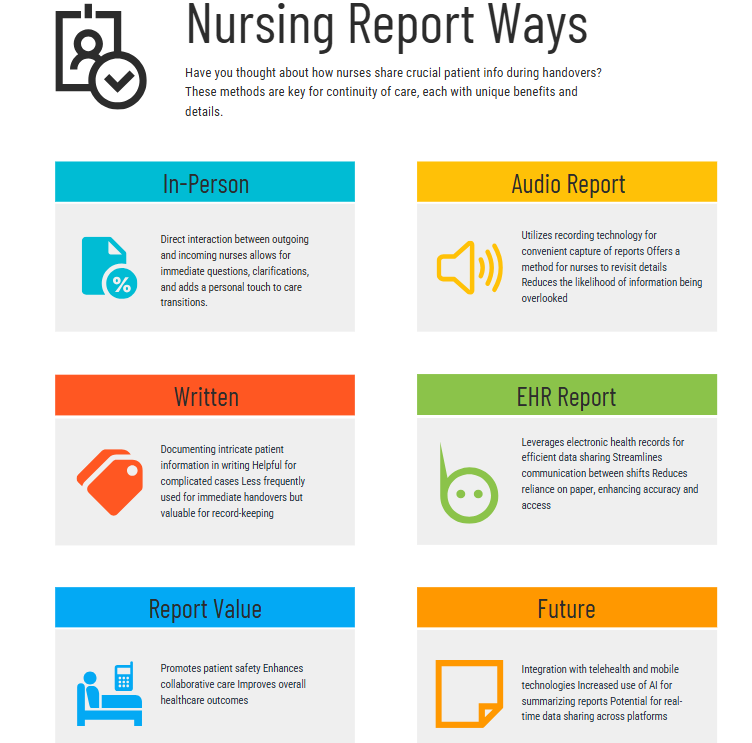
What are the different methods for delivering a nursing report?
The method of delivering a nursing report varies across healthcare settings, but common approaches include:
- Face-to-face report: This traditional method involves a direct conversation between the outgoing and incoming nurse at the bedside or in a designated area. It allows for immediate clarification and detailed discussion.
- Audio-recorded report: This method utilizes technology to record the report, allowing for later review and reducing the risk of information being missed.
- Written report: While less common for real-time handovers, written reports can be useful for documenting specific details or complex patient cases.
- Electronic health record (EHR) based report: Many hospitals now use EHR systems to document and share nursing reports electronically, enhancing efficiency and reducing paperwork.
How can I improve the quality of my nursing report?
Effective communication is key to a successful report for nursing. Here are some tips:
- Be organized and concise: Use a structured approach and avoid unnecessary details.
- Prioritize key information: Focus on significant changes and critical information.
- Use clear and precise language: Avoid medical jargon that might be misunderstood.
- Actively listen and ask clarifying questions: Engage in a two-way conversation to ensure mutual understanding.
- Document everything: Maintain thorough and accurate documentation in the patient’s chart.
- Practice active listening and effective communication skills: This helps ensure that the information is accurately received and understood.
What happens if there are errors or omissions in the nursing report?
Errors or omissions in the nursing report can have serious consequences, potentially leading to adverse patient events. It’s crucial to immediately report any identified inaccuracies or missing information to the appropriate supervisor. This allows for corrective action and prevents potential harm to the patient. Furthermore, thorough documentation of the error, including corrective measures taken, is essential for risk management and quality improvement initiatives.
Continuous learning and feedback mechanisms are vital for refining the nursing report process and ensuring patient safety. Regularly reviewing and improving the nursing report process contributes to a safer and more efficient healthcare environment. By paying attention to detail and using effective communication techniques, nurses can improve the quality of the nursing report and contribute to positive patient outcomes.
Final Remarks
The nursing report is a crucial aspect of patient care, representing a fundamental communication tool within the healthcare system. By following the guidelines outlined in this article, you can hone your skills in writing effective and comprehensive nursing reports. Mastering the art of the report not only enhances the quality of patient care but also contributes to a safer and more efficient healthcare environment. Remember that a well-written report is more than just a record; it’s a vital link in the chain of ensuring optimal patient outcomes.
Proficiency in crafting clear, concise, and comprehensive nursing reports is a testament to a nurse’s commitment to excellence in patient care. The meticulous attention to detail required in creating a high-quality nursing report is vital for maintaining patient safety and ensuring continuity of care. Every nursing report is a testament to the dedication and professionalism of the nursing staff. The nursing report, in its entirety, reflects the commitment to excellence and the dedication to patient well-being that defines the nursing profession.
By understanding and mastering the art of the nursing report, nurses play a crucial role in ensuring safe, effective, and high-quality patient care. The nursing report’s importance cannot be overstated, serving as a vital communication tool and legal document in the ongoing provision of care. Therefore, the ability to write a comprehensive and accurate nursing report is a skill that every nurse must master.
Get Customized Nursing Report Writing Service
At Nursing Papers, we can help you to write authentic nursing reports. Besides report writing, we also do proofreading, editing and formatting to ensure the most comprehensive and accurate reports. Our writers can also assist you in crafting nursing case studies, research papers, essays and dissertations. Get in touch with us today for a customized nursing report writing service!