Table of Contents
The landscape of healthcare is undergoing a profound transformation, driven by technological advancements and evolving patient expectations. At the forefront of this revolution is telehealth and remote care delivery, a multifaceted approach that leverages telecommunications technology to provide healthcare services, support, and education at a distance.
This comprehensive guide discusses the intricacies of telehealth and remote care delivery, exploring its evolution, core components, benefits, challenges, applications, and future trajectory. As healthcare systems worldwide grapple with challenges of accessibility, cost, and quality, understanding the potential and complexities of these innovative care models is more crucial than ever.
The Evolution of Telehealth and Remote Care Delivery
The concept of delivering healthcare remotely is not entirely new. Its origins can be traced back to the early 20th century when radio was used to provide medical advice to ships at sea, and later, in the mid-century, when a few hospitals began experimenting with transmitting medical information, like X-rays, via telephone lines. However, it was the advent of the internet, widespread mobile technology, and high-speed broadband that truly catalyzed the growth of modern telehealth and remote care delivery.
Initially, adoption was gradual, often confined to specific niches like teleradiology or pilot programs in rural areas. The regulatory landscape was complex, and reimbursement policies were often restrictive. However, a confluence of factors began to accelerate its acceptance:
- Technological Maturation: Improved video conferencing quality, secure data transmission protocols, and the proliferation of smartphones and wearable devices made remote interactions more feasible and reliable.
- Growing Consumer Demand: Patients, increasingly accustomed to on-demand services in other sectors, began seeking more convenient and accessible healthcare options.
- Systemic Pressures: Healthcare systems faced mounting pressures to improve efficiency, manage chronic diseases more effectively, and extend care to underserved populations.
- Global Health Events: The COVID-19 pandemic served as an unprecedented catalyst, compelling a rapid and widespread adoption of telehealth and remote care delivery as in-person visits became restricted. This period demonstrated its viability and value on a global scale, overcoming many pre-existing barriers related to adoption and reimbursement.
Core Components of Telehealth and Remote Care Delivery
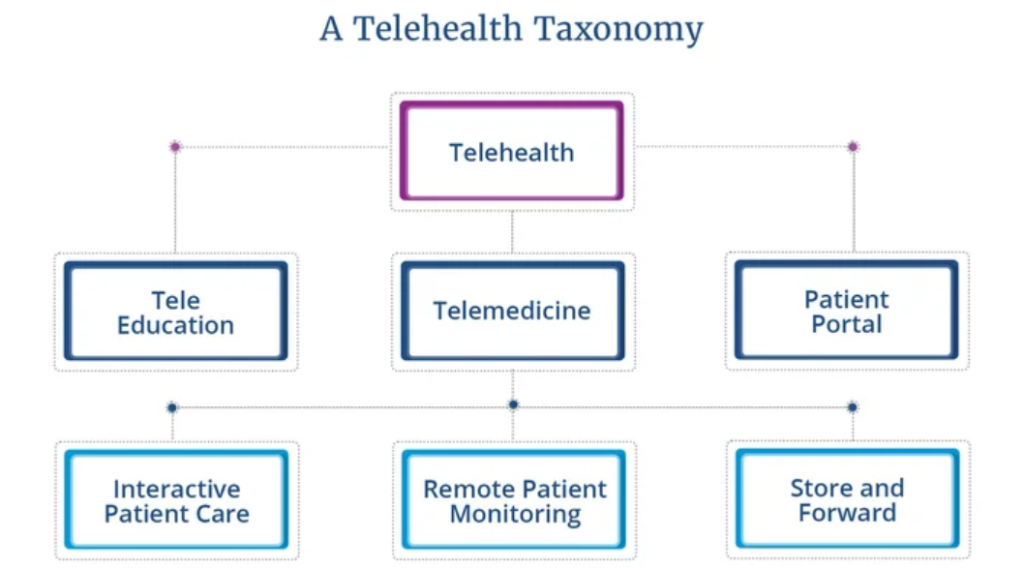
Telehealth and remote care delivery encompasses a broad spectrum of services and technologies. Understanding its core components is essential for appreciating its versatility and potential applications.
Modalities of Delivery
Telehealth services can be broadly categorized based on the timing and nature of the interaction:
- Synchronous (Real-Time) Telehealth: This involves live, two-way interaction between a patient and a healthcare provider, typically via video conferencing or phone call. It is suitable for consultations, assessments, and urgent care needs where immediate feedback is necessary. Examples include:
- Live video consultations with a primary care physician or specialist.
- Virtual therapy sessions.
- Real-time patient education.
- Asynchronous (Store-and-Forward) Telehealth: This involves the collection of medical information (e.g., images, lab results, patient history) which is then transmitted to a provider for review at a later time. The provider reviews the information and responds when available. This is common in specialties like:
- Dermatology (sharing images of skin conditions).
- Radiology (transmitting X-rays or CT scans for interpretation).
- Pathology (sharing digital slides).
- Remote Patient Monitoring (RPM): This component of telehealth and remote care delivery involves using digital technologies to collect health data from patients in one location and electronically transmit that information securely to healthcare providers in a different location for assessment and recommendations. RPM is particularly valuable for:
- Managing chronic conditions like diabetes, hypertension, and heart failure.
- Post-operative monitoring.
- Early detection of health deterioration.
Key Technologies Powering Telehealth and Remote Care Delivery
The successful implementation of telehealth and remote care delivery relies on a robust technological infrastructure:
- Video Conferencing Platforms: Secure, HIPAA-compliant platforms that enable high-quality audio and video interactions.
- Secure Messaging Systems: Encrypted communication channels for non-urgent patient-provider communication, appointment reminders, and sharing of information.
- Wearable Devices and Sensors: Devices like smartwatches, fitness trackers, blood pressure monitors, and glucose meters that collect physiological data for RPM.
- Electronic Health Record (EHR) / Electronic Medical Record (EMR) Integration: Seamless integration with EHR/EMR systems is crucial for continuity of care, allowing providers to access patient history and document virtual encounters.
- Mobile Health (mHealth) Applications: Smartphone apps that facilitate access to telehealth services, manage appointments, track health data, and provide educational resources.
- Digital Diagnostic Tools: Peripherals like digital stethoscopes, otoscopes, and dermatoscopes that can be used by patients (sometimes with assistance) to capture clinical data for remote assessment.
The Myriad Benefits of Telehealth and Remote Care Delivery
The adoption of telehealth and remote care delivery offers a wide array of benefits for patients, providers, and the healthcare system as a whole. These advantages are driving its continued expansion and integration into mainstream healthcare.
Benefits for Patients
- Improved Access to Care: This is perhaps the most significant benefit. Telehealth and remote care delivery can bridge geographical barriers, providing access to specialists and primary care for individuals in rural or remote areas, as well as those with mobility limitations or transportation challenges.
- Convenience and Comfort: Patients can receive care from the comfort of their homes, eliminating the need for travel, time off work, and arranging childcare. This convenience often leads to better adherence to follow-up appointments.
- Reduced Travel Time and Costs: By avoiding physical travel to a clinic or hospital, patients save on transportation expenses (fuel, public transport, parking) and the time associated with commuting and waiting rooms.
- Better Management of Chronic Conditions: RPM allows for continuous monitoring and timely interventions, empowering patients to manage their chronic diseases more effectively and potentially preventing acute exacerbations. The consistent support offered through telehealth and remote care delivery can improve outcomes.
- Enhanced Patient Engagement and Empowerment: Access to personal health data, educational resources, and direct communication channels can empower patients to take a more active role in their healthcare.
- Reduced Exposure to Infections: Virtual visits minimize the risk of exposure to contagious illnesses often present in crowded waiting rooms, a particularly important consideration for immunocompromised individuals or during outbreaks.
Benefits for Providers
- Increased Efficiency and Workflow Optimization: Telehealth and remote care delivery can streamline certain types of appointments, reduce no-show rates, and allow for more flexible scheduling.
- Expanded Reach and Patient Base: Providers can extend their services beyond their immediate geographical vicinity, reaching a larger and more diverse patient population.
- Reduced Overhead Costs: While initial investment in technology is required, telehealth can potentially reduce the need for extensive physical office space and associated operational costs.
- Improved Work-Life Balance: For some providers, the flexibility offered by telehealth and remote care delivery can contribute to a better work-life balance, though this needs careful management to avoid burnout.
- Enhanced Care Coordination: Facilitates easier communication and collaboration among different providers involved in a patient’s care, particularly when integrated with shared EHR systems.
Benefits for the Healthcare System
- Reduced Hospital Readmissions: Effective post-discharge monitoring through RPM and virtual follow-ups can help identify and address potential complications early, reducing costly hospital readmissions.
- Cost-Effectiveness: By improving efficiency, reducing readmissions, and enabling preventative care, telehealth and remote care delivery can contribute to overall cost savings within the healthcare system.
- Better Public Health Surveillance and Response: During public health crises, telehealth platforms can be rapidly scaled to provide screening, triage, and information dissemination, as well as monitor population health trends.
Navigating the Challenges and Considerations in Telehealth and Remote Care Delivery
Despite its numerous advantages, the widespread and effective implementation of telehealth and remote care delivery is not without its challenges. Addressing these hurdles is critical for realizing its full potential.
Technological Barriers
- The Digital Divide: Unequal access to reliable high-speed internet, smartphones, computers, or other necessary devices can create disparities, excluding vulnerable populations from the benefits of telehealth and remote care delivery.
- Digital Literacy: Patients, particularly older adults or those less familiar with technology, may lack the skills or confidence to use telehealth platforms effectively. Provider training is also crucial.
- Interoperability Issues: Lack of seamless data exchange between different telehealth platforms and EHR/EMR systems can create information silos and hinder care coordination.
- Technical Support: Both patients and providers require access to timely technical support to troubleshoot issues with hardware, software, or connectivity.
Regulatory and Reimbursement Hurdles
- Licensing Across State/National Lines: Providers are typically licensed to practice in specific states or regions. Providing care via telehealth and remote care delivery to patients in other jurisdictions can be complicated by varying licensing requirements, although many temporary waivers were issued during the pandemic.
- Varying Reimbursement Policies: Reimbursement rates and coverage for telehealth services can differ significantly across payers (Medicare, Medicaid, private insurers) and can change, creating uncertainty for providers. Parity laws, which mandate equal pay for virtual and in-person services, are not universal.
- Privacy and Security Concerns (HIPAA/GDPR Compliance): Transmitting sensitive patient health information (PHI) electronically requires robust security measures to protect against data breaches and ensure compliance with privacy regulations like HIPAA in the US or GDPR in Europe. Ensuring end-to-end encryption and secure platforms is paramount for any telehealth and remote care delivery service.
Clinical Limitations
- Inability to Perform Physical Exams: A significant limitation of most telehealth and remote care delivery encounters is the inability to conduct a comprehensive hands-on physical examination. This can make diagnosing certain conditions challenging.
- Establishing Patient-Provider Rapport: While many providers and patients report strong connections via telehealth, some find it more difficult to establish the same level of rapport and non-verbal communication as in-person visits.
- Misdiagnosis Concerns: The lack of a physical exam or reliance on patient-reported symptoms can, in some cases, increase the risk of misdiagnosis or delayed diagnosis. Providers must be adept at knowing when an in-person assessment is necessary.
- Appropriateness of Care: Not all conditions or patient needs are suitable for telehealth and remote care delivery. Clear guidelines and clinical judgment are needed to determine when virtual care is appropriate.
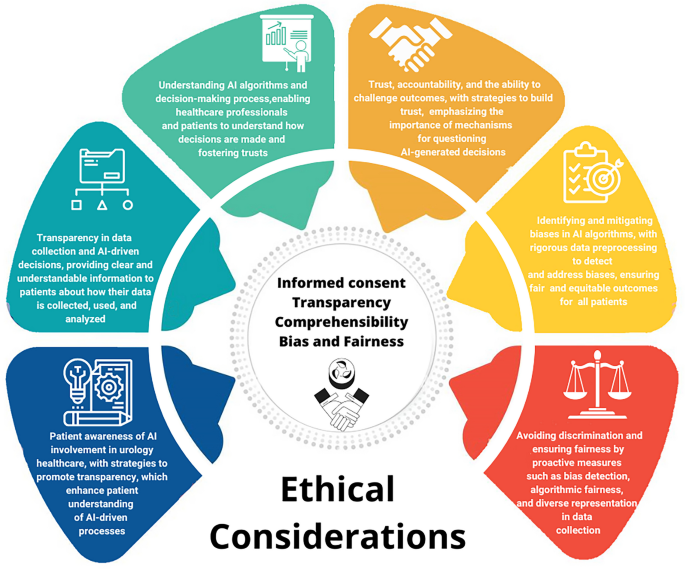
Ethical Considerations
- Equity of Access: Ensuring that telehealth does not exacerbate existing health disparities due to the digital divide or other socioeconomic factors is a critical ethical concern.
- Data Security and Patient Confidentiality: Upholding patient privacy and the security of their health data is fundamental.
- Informed Consent: Patients must be fully informed about the nature of telehealth services, including their benefits, limitations, and potential privacy risks, before consenting to virtual care.
Key Applications of Telehealth and Remote Care Delivery Across Specialties
The versatility of telehealth and remote care delivery allows for its application across a wide range of medical specialties and healthcare settings, transforming how care is delivered.
- Primary Care:
- Routine check-ups for established patients.
- Management of common acute illnesses (e.g., colds, flu, minor infections).
- Medication management and refills.
- Preventive care counseling and health education. This forms a significant portion of modern telehealth and remote care delivery.
- Mental and Behavioral Health:
- Psychotherapy and counseling sessions (individual, group, family).
- Psychiatric evaluations and medication management.
- Substance abuse treatment and support. Telehealth has been particularly transformative in improving access to mental health services.
- Chronic Disease Management:
- Remote monitoring of vital signs (blood pressure, glucose, oxygen saturation) for conditions like diabetes, hypertension, COPD, and heart failure.
- Virtual coaching and support for lifestyle modifications. The continuous engagement facilitated by telehealth and remote care delivery is key.
- Specialist Consultations (Teleconsultations):
- Teldermatology: Patients share images of skin conditions for diagnosis and treatment plans.
- Telecardiology: Remote interpretation of ECGs, monitoring of heart conditions.
- Teleneurology: Stroke assessment (telestroke), follow-up for conditions like Parkinson’s or epilepsy.
- Teleradiology: Transmission and interpretation of medical images by radiologists remotely.
- Post-Operative Follow-Up:
- Virtual check-ins to monitor recovery, assess wound healing (via images), and address patient concerns, reducing the need for burdensome travel.
- Pediatrics:
- After-hours urgent care for common childhood illnesses.
- Behavioral health support.
- Follow-up for certain chronic conditions.
- Obstetrics and Gynecology (TeleOBGYN):
- Prenatal and postpartum check-ins.
- Lactation consulting.
- Contraceptive counseling.
- Rehabilitation Services (Telerehabilitation):
- Remote physical therapy, occupational therapy, and speech therapy sessions.
- School-Based Telehealth: Providing access to healthcare services for students directly within the school setting, connecting them with providers remotely. This application of telehealth and remote care delivery improves student health and reduces absenteeism.
The Future of Telehealth and Remote Care Delivery
The rapid adoption and evolution of telehealth and remote care delivery seen in recent years is just the beginning. The future promises even more sophisticated and integrated virtual care models.
- Integration with Artificial Intelligence (AI) and Machine Learning (ML): AI algorithms can assist in triaging patients, analyzing medical images, predicting disease outbreaks, personalizing treatment plans, and powering chatbots for initial patient interactions.
- Advancements in Wearable Technology and RPM: Expect more sophisticated, less intrusive, and more accurate wearable sensors that can monitor a wider range of physiological parameters continuously, providing richer data for proactive care.
- Expansion into New Clinical Areas: As technology improves and evidence of efficacy grows, telehealth and remote care delivery will likely expand into more complex areas of care, including more intensive remote monitoring and even support for certain remote procedures.
- Greater Emphasis on Personalized and Predictive Medicine: The vast amounts of data collected through telehealth and RPM, when analyzed effectively, can lead to more personalized healthcare interventions and predictive models that identify at-risk individuals before serious health issues arise.
- Hybrid Care Models: The future is unlikely to be exclusively virtual or in-person. Instead, hybrid models that seamlessly blend the strengths of both will become the norm, with care pathways designed to utilize telehealth and remote care delivery where it is most effective and appropriate.
- Enhanced Virtual Reality (VR) and Augmented Reality (AR) Applications: VR and AR could be used for immersive patient education, surgical training, remote consultations with enhanced visualization, and even therapeutic interventions (e.g., pain management, phobia treatment).
- Improved Interoperability and Data Sharing: Continued efforts towards standardized data formats and secure health information exchange will be crucial for realizing the full potential of integrated care.

Research and Academic Perspectives on Telehealth and Remote Care Delivery
The rapid expansion of telehealth necessitates ongoing research to evaluate its effectiveness, safety, cost-efficiency, and impact on health equity. Academics and healthcare professionals play a vital role in building the evidence base for telehealth and remote care delivery. Writing a comprehensive research paper about telehealth and remote care delivery can contribute significantly to understanding best practices, identifying areas for improvement, and guiding policy decisions.
In nursing, the implications are particularly profound. Nurses are often at the forefront of implementing and managing telehealth services, from conducting virtual visits to educating patients on RPM devices. A nursing paper about telehealth and remote care delivery might explore topics such as patient experiences, nurse satisfaction, workflow adaptations, or the impact on chronic disease management from a nursing perspective.
For students and researchers navigating these complex topics, resources like academic paper writing services can offer support in structuring research, analyzing data, and disseminating findings effectively, ensuring that high-quality evidence continues to shape the evolution of these care models. In case you need help with assignments, term papers, essays, research papers, case studies, thesis and dissertations, do not hesitate to engage Nursing Papers. Our service covers topic suggestion, paper writing, proofreading, editing, formatting and plagiarism removal.
Implementing a Successful Telehealth and Remote Care Delivery Program
Successfully launching and sustaining a telehealth and remote care delivery program requires careful planning, strategic execution, and continuous adaptation. Key steps include:
- Needs Assessment: Identify the specific needs of your patient population and organization. Which services are most suitable for remote delivery? What are the goals of the telehealth program?
- Technology Selection: Choose user-friendly, secure, and HIPAA-compliant platforms that integrate with existing systems like EHRs. Consider scalability and technical support.
- Develop Clear Workflows and Protocols: Define processes for scheduling, conducting virtual visits, documentation, billing, and handling technical issues or emergencies.
- Staff Training and Buy-in: Comprehensive training for all staff (clinical and administrative) is essential. Address concerns and ensure buy-in by highlighting the benefits.
- Patient Education and Onboarding: Educate patients on how to use the telehealth platform, what to expect during a virtual visit, and how their privacy will be protected. Provide clear instructions and support.
- Establish Key Performance Indicators (KPIs): Track metrics such as patient satisfaction, provider satisfaction, no-show rates, clinical outcomes, and cost-effectiveness to evaluate the program’s success.
- Continuous Evaluation and Improvement: Regularly review program performance, gather feedback from patients and staff, and make necessary adjustments to optimize the service. The landscape of telehealth and remote care delivery is dynamic, requiring ongoing adaptation.
Conclusion
Telehealth and remote care delivery has firmly established itself as an indispensable component of modern healthcare. Its ability to enhance access, improve convenience, support chronic disease management, and increase efficiency is undeniable. While challenges related to technology, regulation, and equity persist, ongoing innovation, supportive policies, and a commitment to patient-centered care are paving the way for its continued growth and integration.
The journey of telehealth and remote care delivery is far from over; it is an evolving field that promises to further reshape how healthcare is accessed and experienced, ultimately aiming for a more connected, responsive, and equitable health system for all. The future is bright for telehealth and remote care delivery, and its role in transforming global health is only set to expand.