Table of Contents
The healthcare landscape is constantly evolving, and telemetry nursing plays a pivotal role in this transformation. By leveraging technology, telemetry nurses remotely monitor patients’ vital signs, ensuring timely intervention and improved outcomes. This guide delves into the world of telemetry nursing, exploring its core functions, advanced applications, and the exciting future it holds.
Introduction to Telemetry Nursing
Telemetry nursing utilizes technology to continuously monitor patients’ vital signs from a central location. Unlike traditional bedside monitoring, telemetry allows for greater patient mobility and flexibility within the healthcare setting. The evolution of telemetry technology has revolutionized patient care, enabling healthcare providers to keep a watchful eye on patients even beyond the confines of a hospital room.

The benefits of telemetry nursing are multifaceted. Patients experience improved comfort and potentially shorter hospital stays. Healthcare providers, on the other hand, benefit from increased efficiency, allowing them to manage a larger patient load effectively. Additionally, telemetry nursing facilitates early intervention by enabling healthcare professionals to identify potential complications before they escalate.
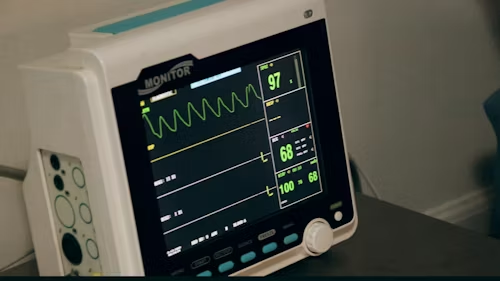
Telemetry primarily focuses on monitoring various physiological parameters. Electrocardiogram (ECG) waveforms, which provide vital information about heart rhythm and electrical activity, are a cornerstone of telemetry nursing. But the scope extends beyond the heart. Respiratory rate, blood oxygen saturation (SpO2), and blood pressure are also commonly monitored using telemetry devices.
Understanding Telemetry Equipment
Telemetry systems come in various forms to cater to different patient needs. Transmitter patches and leads, connected to electrodes placed on the chest, are the workhorses of telemetry nursing for continuous ECG monitoring. For extended ECG monitoring beyond the hospital setting, telemetry nurses may utilize Holter monitors. Pulse oximeters, worn on the fingertip, are another essential tool in a telemetry nurse’s arsenal, providing real-time data on blood oxygen saturation. Automated blood pressure cuffs complete the picture, offering periodic measurements for telemetry nurses to integrate into their assessments.
The successful application of telemetry hinges on proper equipment usage. Telemetry nurses play a crucial role in selecting the appropriate telemetry systems based on the specific needs of each patient. Meticulous placement of electrodes and sensors is paramount for accurate data collection. Telemetry nurses ensure patient comfort and safety by securing the equipment appropriately while maintaining its functionality. Troubleshooting common technical issues with telemetry devices also falls within the purview of a skilled telemetry nurse.
Core Functions of a Telemetry Nurse

Continuous patient monitoring is the bedrock of telemetry nursing. Telemetry nurses become adept at interpreting real-time data streams, analyzing ECG waveforms for signs of arrhythmias, and monitoring trends in vital signs like respiratory rate, SpO2, and blood pressure. Identifying even subtle abnormalities in these parameters allows for early intervention, potentially preventing serious complications. Telemetry nurses meticulously document their observations and trends within patient charts, creating a comprehensive picture of the patient’s condition.
Responding to critical events is another critical responsibility of telemetry nurses. Recognizing signs and symptoms of patient deterioration, such as chest pain, shortness of breath, or abnormal vital signs on the telemetry system, demands immediate action. Telemetry nurses must be well-versed in established protocols for responding to emergencies. Alerting physicians and other healthcare professionals promptly ensures a coordinated response to critical situations. In some cases, depending on their training and facility protocols, telemetry nurses may be required to provide basic life support measures until advanced medical help arrives.
Patient education and communication are integral aspects of effective telemetry nursing. Telemetry nurses explain the purpose and function of telemetry monitoring to patients, alleviating any anxieties they might have about the equipment. Addressing patient concerns and fostering open communication is key to ensuring patient cooperation and a smooth monitoring process. Telemetry nurses also play a vital role in encouraging patients to report any discomfort or changes in their condition, which could be early signs of potential complications. Maintaining clear and concise communication with physicians and other healthcare team members ensures a collaborative approach to patient care.
Advanced Applications of Telemetry Nursing
The reach of telemetry nursing extends beyond the walls of traditional hospital settings. Telemetry has become a valuable tool in home care settings, allowing for the remote monitoring of chronically ill patients or those recovering from surgery. Telemetry nurses can monitor vital signs remotely, identifying potential complications early on and preventing unnecessary hospital admissions. This not only improves patient outcomes but also enhances patient independence and quality of life.

Critical care units heavily rely on telemetry for continuous monitoring of critically ill patients. Real-time data from telemetry systems enables healthcare professionals to detect life-threatening events such as sepsis, shock, or cardiac arrest at their earliest stages. Early detection allows for rapid intervention and potentially life-saving measures. This emphasis on early intervention extends beyond critical care units. Telemetry plays a crucial role in telemedicine, which leverages telecommunication technology to facilitate remote consultations between patients and healthcare providers. Integration of telemetry data into these consultations empowers healthcare professionals to make informed decisions about a patient’s care plan, even when not physically present. This technology is particularly beneficial for patients in remote locations, where access to specialized healthcare services might be limited.
Expanding Your Telemetry Nursing Expertise (800 words)
This guide has provided a solid foundation for understanding telemetry nursing. To further equip you for success in this dynamic field, let’s delve deeper into some key areas:
Understanding Electrocardiogram (ECG) Waveforms:
ECG is the cornerstone of telemetry monitoring. It provides a visual representation of the electrical activity of the heart throughout a cardiac cycle. Interpreting these waveforms is a crucial skill for telemetry nurses. Common ECG components you’ll encounter include:
- P Wave: Represents atrial depolarization (contraction)
- PR Interval: Time taken for the electrical impulse to travel from the atria to the ventricles
- QRS Complex: Represents ventricular depolarization
- ST Segment: Reflects the period between ventricular depolarization and repolarization
- T Wave: Represents ventricular repolarization
Telemetry nurses must be able to identify normal ECG patterns and recognize deviations that might indicate arrhythmias. Some common arrhythmias monitored through telemetry include:
- Premature Atrial Contractions (PACs): Early heartbeats originating from the atria.
- Premature Ventricular Contractions (PVCs): Early heartbeats originating from the ventricles.
- Atrial Fibrillation (AFib): Irregular heart rhythm due to disorganized electrical activity in the atria.
- Ventricular Tachycardia (VT): Fast heart rhythm originating from the ventricles.
Beyond ECG: Advanced Telemetry Parameters
While ECG remains central, telemetry systems offer a broader range of monitoring capabilities:
- Respiratory Rate: Monitored through chest impedance or pulse oximetry, changes in respiratory rate can indicate potential respiratory distress.
- Blood Oxygen Saturation (SpO2): Measured by pulse oximeters, SpO2 reflects the percentage of oxygen-carrying hemoglobin in the blood. Low SpO2 can signify respiratory problems.
- Blood Pressure: Automated blood pressure cuffs provide periodic measurements for telemetry nurses to assess for hypertension or hypotension.
- Temperature: In some cases, telemetry systems may integrate temperature monitoring to identify potential infections.
Alarm Management in Telemetry Nursing
Telemetry systems generate alarms to alert nurses of potential abnormalities. However, excessive alarms can lead to “alarm fatigue,” where nurses become desensitized to the constant alerts. To address this, telemetry nurses need to adopt effective alarm management strategies:
- Prioritize Alarms: Distinguish between critical and non-critical alarms based on the severity of the potential issue.
- Investigate Promptly: Respond to alarms quickly to assess the situation and determine if intervention is necessary.
- Document Actions: Meticulously document your response to each alarm in the patient’s chart for clear communication and future reference.
- Collaboration is Key: Work with physicians to establish appropriate alarm settings and protocols for optimal patient care.
Special Considerations in Telemetry Nursing
Certain patient populations require specific considerations in a telemetry setting:
- Cardiac Post-Operative Patients: Close monitoring of ECG for arrhythmias and vital signs to ensure proper recovery after heart surgery.
- Patients with Pacemakers/Defibrillators: Telemetry nurses need to understand the specific device function and monitor for potential malfunctions.
- Patients with Chronic Conditions: Telemetry can be valuable for monitoring patients with chronic heart failure, COPD, or other conditions that can impact vital signs.
The Ethical Considerations of Telemetry Nursing
Telemetry nursing raises important ethical considerations:
- Patient Privacy: Maintaining patient confidentiality and data security is paramount when handling sensitive health information collected through telemetry.
- Informed Consent: Patients have the right to understand the purpose of telemetry monitoring and provide informed consent before its use.
- End-of-Life Care: Decisions regarding the continued use of telemetry in end-of-life situations should be made with sensitivity and respect for patient autonomy and family wishes.
Conclusion: A Rewarding Career Path
Telemetry nursing offers a dynamic and intellectually stimulating career path for nurses who thrive in a technology-driven environment. By mastering telemetry skills, you become a valuable asset to the healthcare team, playing a vital role in ensuring patient safety and improving outcomes.
Remember, continuous learning is essential in this ever-evolving field. Explore the resources mentioned earlier, stay updated on the latest advancements in telemetry technology, and consider pursuing additional training or certifications to enhance your expertise. With dedication, you can become a leader in telemetry nursing, contributing to the future of patient care and shaping the trajectory of this exciting field.
The Future of Telemetry Nursing
The future of telemetry nursing is brimming with exciting possibilities. Advancements in telemetry technology are paving the way for even more sophisticated patient monitoring. Wearable and implantable monitoring devices offer the potential for continuous data collection, providing a more comprehensive picture of a patient’s health. Artificial intelligence (AI)-powered algorithms are being developed to analyze telemetry data automatically, enabling real-time anomaly detection and potentially revolutionizing how healthcare professionals respond to critical situations. Data security and privacy remain paramount concerns, and advancements in these areas will be crucial for the continued success of telemetry nursing.
The impact of these advancements will undoubtedly reshape nursing practice. The demand for telehealth-skilled nurses with expertise in interpreting telemetry data is expected to rise significantly. Telemetry nursing fosters enhanced collaboration between nurses and other healthcare professionals across geographical boundaries, leading to a more holistic approach to patient care. The integration of continuous patient monitoring with AI-powered analysis has the potential to pave the way for personalized medicine, with treatment plans tailored to an individual’s unique health profile.
Conclusion
Telemetry nursing has become an indispensable tool in modern healthcare, offering a multitude of benefits for both patients and healthcare providers. It empowers nurses to remotely monitor vital signs, facilitating early intervention and improved patient outcomes. As telemetry technology continues to evolve, the future of telemetry nursing promises even greater advancements in patient care, remote monitoring capabilities, and personalized medicine. For nurses seeking a dynamic and evolving field, telemetry nursing offers a rewarding career path at the forefront of technological innovation in healthcare.
Ready to unlock the potential of Telemetry Nursing? This comprehensive guide has equipped you with the foundation. Now, it’s time to take the next step!
- Bookmark this article as a handy reference for telemetry concepts and best practices.
- Share this guide with fellow nursing students interested in exploring Telemetry Nursing.
- Dive deeper into the recommended resources to hone your telemetry expertise.
- Consider contacting us if you need support with Telemetry Nursing assignments.
Become a confident Telemetry Nurse! With the knowledge gained from this guide and the additional resources, you’re well on your way to a successful career in this dynamic field.